The first extracorporeal shock wave lithotripsy (ESWL) for the destruction or renal stones was performed in 1981 and was published in a paper including 72 patients.1 There were no complications or changes in renal function, the method was used successfully in all patients with renal pelvic stones, and two patients with ureteral stones had to be operated on because of insufficient stone destruction.
There are many factors that can reduce the stone-free rates following ESWL. These can be divided into the patient, stone, and technical factors, as seen in figure 1.
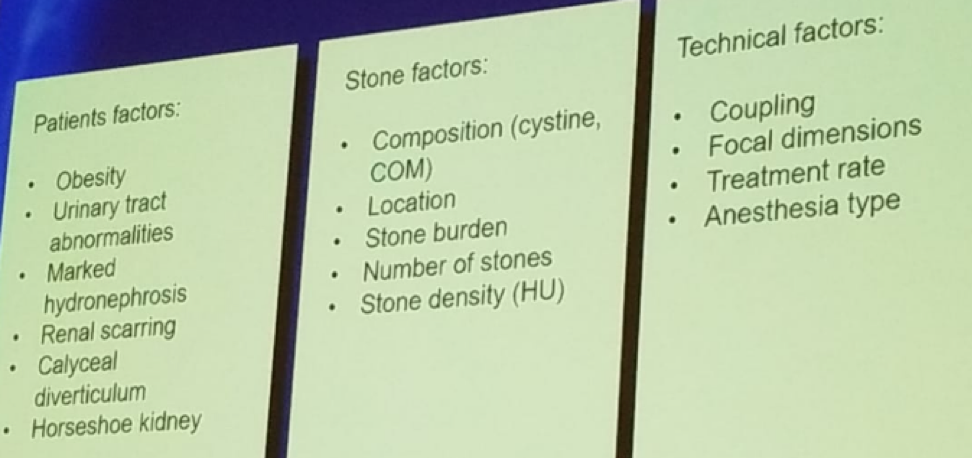
Figure 1- Factors reducing stone-free rate following ESWL:
According to the current American Urology Association (AUA) guidelines, for stone burden less than 20 mm, which is not in the lower pole, the treatment recommendation is either with ESWL or with ureteroscopy (strong recommendation, evidence level grade B). However, ureteroscopy is associated with a lower risk of repeat procedure, and the stone-free status is achieved faster than with ESWL. The advantages of ESWL include its non-invasiveness, patient preference, and lack of stent at the end of the procedure. Whatever procedure is chosen, it is important that this process be a shared decision making one. Ureteroscopy achieves a stone-free rate of around 95% for stones smaller than 2 cm.2 This increases to 100% for stones <1 cm. The most common complications attributable to ureteroscopy include stent symptoms in 11% of patients, transient fever in 2.2% and transfusion rate of 0.7%. Grade 4 Clavien Dindo complications occur only when ureteroscopy is performed for stone sizes of 3 cm or more.3
For stone burden of over 20 mm, the AUA guidelines recommend performing percutaneous nephrolithotomy (PCNL). If the patient is not a good candidate for PCNL, the AUA guidelines recommend a staged ureteroscopy procedure (moderate recommendation, evidence level grade C). These patients include those with a PCNL-incompatible body habitus, variant renal anatomy, or a patient who is anticoagulated. Holmium-laser ureteroscopy has been proven to be safe and effective in anticoagulated patients.4 Indications for ureteroscopy for stones larger than 2 cm include:
- Obesity
- Anticoagulation
- Skeletal deformity
- Other medical comorbidities
- Patient preference
- Concomitant ureteral stone
- Failed PCNL access
- Renal anomalies
A systematic review including 7 studies with 131 patients treated with ureteroscopy has shown that it is a safe procedure for obese patients. 5 Ureteroscopy has also been shown to be safe and most effective in patients with renal anomalies, including horseshoe kidney, ectopic kidney, and malrotated kidney. The ureteral stone-free rate was 85%, 94, and 88%, respectively, while the renal stone-free rate was 77%, 20%, and 71%, respectively.
Dr. Denstedt concluded his talk with a few words on what the future holds for this growing field. It is almost certain, that digital endoscopes will dominate the field. These entail 9.3-8.7 Fr tapered shaft, with a 3.6 Fr working channel, with 250-degree deflection, 80-degree field of view, demonstrating a larger image with no camera. We will also see the use of disposable flexible ureteroscopies that eliminate the need to be concerned with their fragility. These disposable ureteroscopies will be dynamic, digital and reliable. In a study performing micro-cost analysis, the costs of the disposable and reusable ureteroscope were comparable.6 In a systematic review of the single-use flexible ureteroscopy, 11 studies with 466 patients were included. The authors concluded that no difference in procedure duration, stone-free rate, or complications were witnessed when compared to the standard reusable ureteroscope.7
Presented by: John Denstedt, MD, Western Ontario University, Canada
References:
1. Chaussy C et al. J Urol 1981
2. Hyams ES et al. J Urol 2015
3. Al-Qahtani SMAI et al.EAU 2013
4. Watterson JD et al. J Urol 2002
5. Aboumarzouk OM et al. BJU Int. 2012
6. Taguchi K et al. J of Endo 2018
7. Davis NF et al. World J. Urol 2018
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, @GoldbergHanan at the 70th Northeastern Section of the American Urological Association (NSAUA) - October 11-13, 2018 - Fairmont Royal York Toronto, ON Canada


