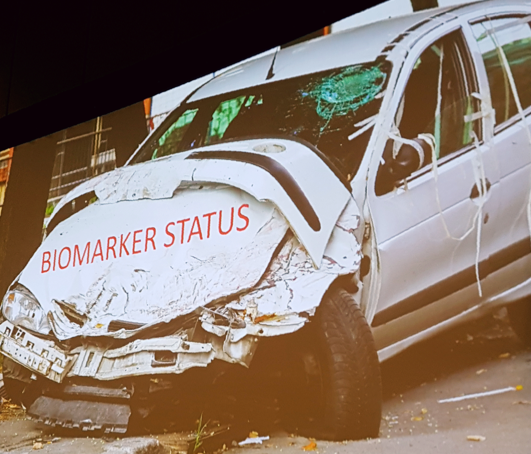
Davies posed the question “are urologists using biomarkers”? In a Twitter survey of 240 respondents, 75% reported that biomarkers were not needed, 7% used Decipher, 8% used Prolaris, and 10% used ConfirmDx. Davies notes that indeed, it appears that urologists are not using biomarkers, showing the fiscal first-quarter 2018 Revenue By Product stats that YoY growth from 1Q17 to 1Q18 was 0% for Prolaris.
Davies highlights that over the last year we have two studies (PRECISION1 and PROMIS2) that suggest that men with an increased PSA should have an mpMRI prior to prostate biopsy. As deftly highlighted, in the PROMIS study, there were 0 cases of Gleason ≥4+3 prostate cancer missed by mpMRI. Long-term active surveillance outcomes suggest that 15-year prostate cancer specific mortality (PCSM) incidence for strict criteria (no Gleason 3+4) is 0.1% and 5.7% for expanded criteria (some Gleason 3+4). Metastasis incidence for strict AS criteria is 0.1% and 2.8% for expanded criteria. So even when patients are enrolled in active surveillance programs, Davies asks “do we really need to biomarkers” when mortality and PCSM outcomes in these patients are so low?
Davies highlights that there are four components that should encompass the perfect biomarker:
- Developed in active surveillance patients
- Validated in active surveillance patients
- Improve prostate mortality
- Decreases metastatic rate
- Prognostic flaws – GPS has a minor improvement in stratification, but in a low-risk cohort, the AUC only improved to 0.67 from 0.63 (clinical only). Furthermore, Prolaris fails to improve prognostication without clinical input.
- Imaging flaws – in a study evaluating the association between GPS and mpMRI, mean GPS results differed between mpMRI categories (p=0.001), however, a broad range was observed for all categories, particularly for Gleason 3+4 disease3.
- Basic science flaws – in data provided to Davies by colleagues at the University of Michigan, there is a demonstration of clonal independence among biopsy sampled prostates.
Presented by: Ben Davies, MD, University of Pittsburgh
Read the Opposing Debate: Biomarker Debate: Adopt, Expand, Trust (PRO)
References:
- Ahmed HU, El-Shater Bosaily A, Brown LC, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): A paired validating confirmatory study. Lancet 2017;389(10071):815-822.
- Kasivisvanathan V, Rannikko AS, Borghi M, et al. MRI-targeted or standard biopsy for prostate cancer diagnosis. N Engl J Med 2018;378(19):1767-1777.
- Leapman MS, Westphalen AC, Ameli N, et al. Association between a 17-gene genomic prostate score and multi-parametric prostate MRI in men with low and intermediate risk prostate cancer (PCa). PLoS One 2017;12(10):e0185535.


