For this study, the authors retrospectively assessed the records of 200 consecutive patients who underwent preoperative mpMRI and radical prostatectomy from 2011 to 2015 at a single institution. Patients were excluded if they received neoadjuvant androgen deprivation therapy or whose pathological diagnosis was ≥pT2. To classify tumors as anterior or posterior, the authors defined the largest lesion as the index tumor if there were several masses. The correlation between MRI tumor contact length and microscopic extracapsular extension in the radical prostatectomy specimen was evaluated by developing probability plots of extracapsular extension versus tumor contact length.
Among these 200 patients, 47% (n=95) had an anterior tumor and 105 patients (53%) had a posterior tumor. The anterior tumor group had a higher initial PSA (≥10 ng/ml, 24% vs. 16%, p=0.005) and lower pathological Gleason score (≤3+4, 51% vs. 41%, p=0.01) compared to the posterior tumor group. Postoperative pathological analysis confirmed pT3 in 12 patients (13%) with an anterior tumor versus 44 patients (42%) with a posterior tumor. In all patients, the tumor contact length of the suspected lesion on MRI corresponded to the index tumor in the pathological specimen, ranging from 0 cm (no contact) to 5.2 cm. The probability plots of extracapsular extension versus tumor contact length demonstrated that anterior tumors were less likely to invade the extracapsular tissues:
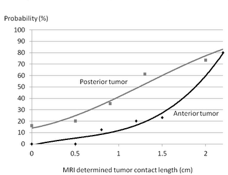
Among patients whose tumor contact length was 1.0-1.5 cm, 20% of patients with an anterior tumor had extracapsular extension compared to 57% of patients with a posterior tumor (p=0.02).
The strength of this study is consecutive patient’s enrolled in the study reducing the risk of selection bias. These results will be useful for preoperative radical prostatectomy planning and clarifying patients that are ineligible for possible focal therapy. A possible limitation is the small overall sample size, thus reducing the number of pT3 events and precluding multivariable analysis for predictors of pT3 in this cohort. Based on Dr. Matsumoto’s findings, he concluded that anterior tumors have more favorable pathological characteristics than posterior tumors with the same MRI contact length. When setting the optimal threshold for tumor contact length to predict microscopic extracapsular extension, we have to consider tumor location in the prostate.
Presented by: Kazuhiro Matsumoto, Keio University School of Medicine, Tokyo, Japan
Co-Authors: Kimiharu Takamatsu, Seiya Hattori, Toshikazu Takeda, Takeo Kosaka, Ryuichi Mizuno, Eiji Kikuchi, Hiroshi Asanuma, Mototsugu Oya, Tokyo, Japan
Written by: Zachary Klaassen, MD, Urologic Oncology Fellow, University of Toronto, Princess Margaret Cancer Centre, Twitter: @zklaassen_md, at the 2018 AUA Annual Meeting - May 18 - 21, 2018 – San Francisco, CA USA


