The study included 537 patients who received SRT at PSA level >0.5 ng/ml. All patients received local radiation to the prostate and seminal vesicle bed at seven tertiary referral centers, whereas the irradiation of the pelvic lymph nodes area (WPRT) and the concomitant hormonal therapy (HT) administration was left at the discretion of the treating physician. The study outcome was clinical recurrence (CR) after SRT that was identified by imaging. Multivariable Cox regression analysis was used to identify significant predictors of CR.
Overall, 475 (88%) patients received SRT for PSA rising during follow-up after RP, whereas 62 (12%) patients were treated for PSA persistence after surgery. Median PSA level at SRT was 1.0 ng/ ml (IQR: 0.7, 1.7). At a median follow-up of 72 months, 102 (19%) patients developed CR. Multivariable analysis demonstrated that pT stage >=pT3b (HR: 4.91, p0.5 ng/ml, SRT was noted to be associated with better outcomes when administered at PSA level at SRT (HR: 1.22, p=0.0017), time from RP to RT (HR: 0.99, p=0.048), WPRT administration (HR: 0.45, p=0.031) and concomitant HT (HR: 0.48, p=0.017) were significant predictors of CR. When the
multivariable risk of CR was plotted against PSA level at SRT, a linear relationship was observed initially, but reached a plateau at 3.0 ng/ml (for patients with PSA rising after RP), and at 2.0 ng/ml (for patients with PSA persistence after RP) (Figure 1).
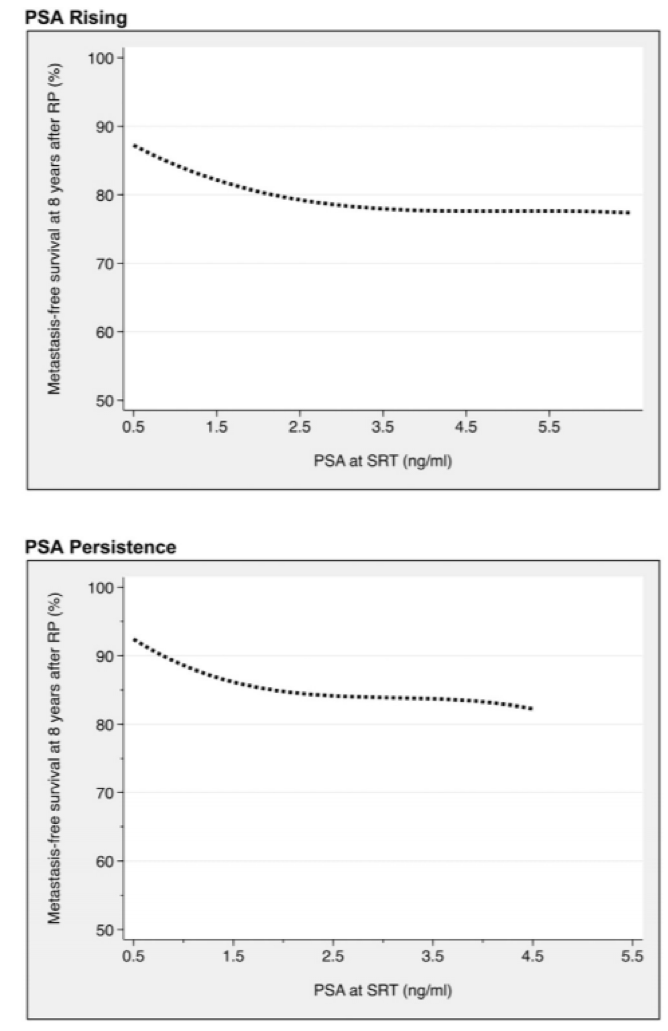
In conclusion, in patients with PSA level >0.5 ng/ml, SRT was noted to be associated with better outcomes when administered at PSA <3.0 ng/ml (for patients with PSA rising after RP), and at PSA <2.0 ng/ml (for patients with PSA persistence after RP). When PSA level exceeds these values, SRT did not show a clear benefit.
Presented by: Nicola Fossati, Milan, Italy
Co-Author: Jeffrey R. Karnes, Matteo Soligo, Stephen A. Boorjian, Rochester, MN, Alberto Bossi, Gabriele Coraggio, Villejuif, France, Nadia Di Muzio, Claudio Fiorino, Cesare Cozzarini, Barbara Noris Chiorda, Giorgio Gandaglia, Milan, Italy, Detlef Bartkowiak, Volker Budach, Ulm, Germany, Shahrokh F. Shariat, Gregor Goldner, Vienna, Austria, Antonino Battaglia, Steven Joniau, Karin Haustermans, Geert De Meerleer, Leuven, Belgium, Valérie Fonteyne, Piet Ost, Ghent, Belgium, Hein Van Poppel, Leuven, Belgium, Francesco Montorsi, Milan, Italy, Thomas Wiegel, Ulm, Germany, Alberto Briganti, Milan, Italy
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 2018 AUA Annual Meeting - May 18 - 21, 2018 – San Francisco, CA USA


