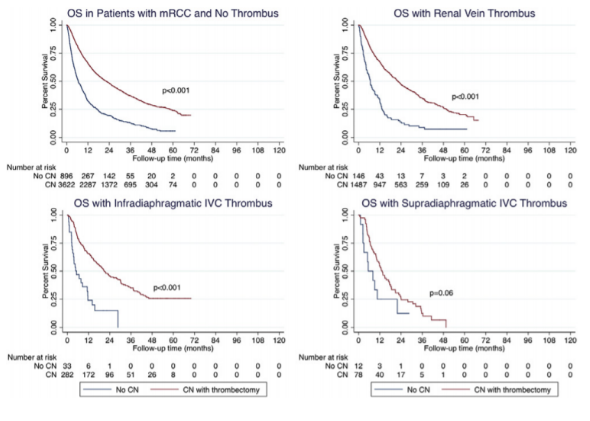
In total, 10521 patients were found to have mRCC during the study period. Approximately 24% had tumor thrombi including 1959 (19%) with renal vein thrombus, 399 (4%) with infradiaphramatic IVC thrombus, and 129 (1%) with supradiaphragmatic IVC thrombus (Figure 1). Median Followup was 10.2 months (3.6-24.3). The one year overall survival for patients with Mrcc and np tumor thrombus, renal vein thrombus, infradiaphragmatic IVC, and supradiaphragmatic IVC tumor thrombus was 71%, 65%, 61% and 51% respectively. CN significantly improved OS for patients with no tumor thrombus (p<0.01), renal vein thrombus (p<0.01), and infradiaphragmatic IVC thrombus (p<0.01). No overall survival benefit was observed in patients who underwent CN with supradiaphragmatic IVC thrombus compared with patients who did not receive CN (p=0.08).
Independent predictors of CN in this cohort included treatment at an academic/research facility, East Central US region, non-clear cell histology, high-grade disease, concurrent metastasectomy, and more recent year of treatment. Patients with T3b and T3c were significantly less likely to undergo CN than patients with T3a disease. Matched Kaplan- Meier curves are shown in Figure 2. On multivariable analysis controlling for patient and tumor specific variables, CN was associated with improved OS (HR 0.36, 95% CI: 0.31-0.42, p<0.001) in patients with mRCC and tumor thrombi. However, this effect was limited to those with T3a (HR 0.34, 95% CI: 0.29-0.41, p<0.01) and T3b (HR 0.31, 95% CI: 0.20-0.50, p<0.01) disease, but not T3c (HR 0.62, 95% CI: 0.31-1.21, p=0.16) disease.
The authors therefore concluded that tumor thrombus is common in patients with mRCC. OS for this patient population is poor and various factors in- fluence the use of CN, including clinic-demographic and tumor specific variables. Despite discrepancies in utilization, CN is associated with improved OS, although this effect appears to be limited in patients with mRCC and tumor thrombus limited to the renal vein and infradiaphragmatic IVC.

Figure 2: Kaplan Meier curves:
Presented By: Andrew Lenis, LA, CA, USA
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre Twitter: @GoldbergHanan at the 2018 AUA Annual Meeting - May 18 - 21, 2018 – San Francisco, CA USA


