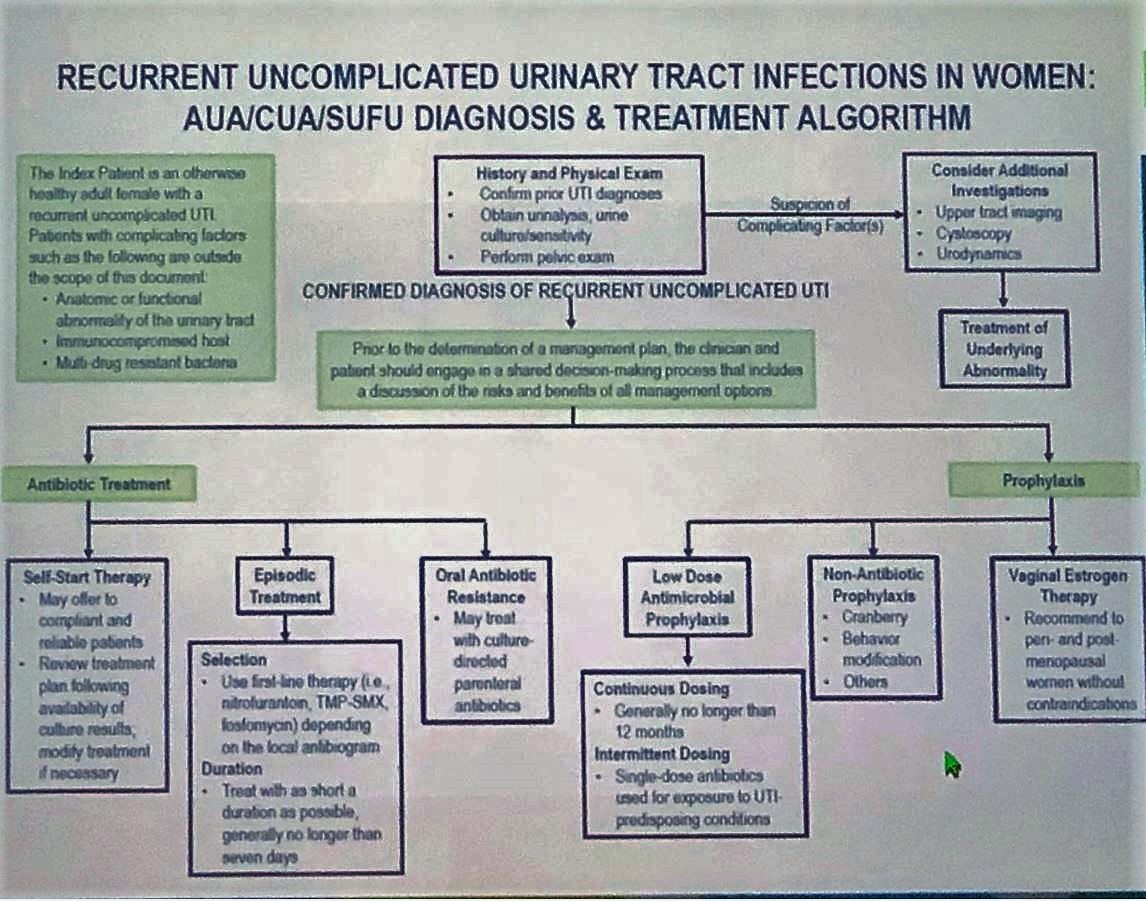
The first case looked at a 25-year-old woman with rUTI who reported recurrent episodes of dysuria and hematuria 1-2 days after intercourse. She usually receives antibiotic from the Urgent care based on her urine culture results, which usually detect >100,000 CFU E. coli. Per Guideline 1, it was recommended to obtain a complete patient history and perform a pelvic exam that was considered normal. However, the patient remembered a history of pediatric urologic surgery involving an X-ray and a catheter. Per Guideline statement 4, the panel expert did not recommend cystoscopy and upper tract imaging. Recurrent uncomplicated UTI treatment algorithm was introduced (Figure 1)
Figure 1
The patient is interested in conservative methods to prevent future recurrences. She’s recommended wiping front to back, showering after sex, and increased hydration. Guideline statement 13 states that clinicians may recommend cranberry prophylaxis for rUTIs, however, there is no data to confirm that other supplements can act as effective preventative measures.
In 2 months case patient reports dysuria and hematuria after intercourse, but no fever, chills, or flank pain. Per guideline statement 15, urinalysis and urine culture and sensitivity has to be obtained with each symptomatic acute cystitis episode prior to starting a treatment regimen. Guideline statement 9 recommends prescribing first-line therapy (nitrofurantoin, TMP-SMX, fosfomycin) for the treatment of symptomatic UTIs in women dependent on a local antibiogram (Figure 2). Per Guideline statement 10, it is recommended to treat rUTIs with a short course of antibiotics, generally no longer than 7 days.
Figure 2

Antibiotic prophylaxis could be prescribed to the rUTI patients following discussion of the risks, benefits, and alternatives (Figure 3).
Figure 3

The second case reflected guideline statements related to the required documentation of positive urine cultures associated with prior symptomatic episodes, repeat urine studies when the initial sample is suspect for contamination and consequent consideration for obtaining a catheterized urine sample and need to repeat urine culture if the patient becomes symptomatic following antimicrobial therapy.
The third case of a post-menopausal woman with a history of rUTIs and vaginal dryness highlighted Guideline statement 7, which states that surveillance urine testing including urine culture should be omitted if the patient is asymptomatic. In addition, clinicians should recommend vaginal estrogen therapy to reduce the risk of future UTIs.
Panel moderator stressed the importance of cultures for the diagnosis, appropriate prevention pathways, treatment and monitoring of rUTIs. Treatment should use shorter courses of antibiotic with minimal collateral damage. Antibiotic prophylaxis is preferred if UTIs continue to recur, and management should be focused on alleviating symptoms, preventing a recurrence, and reducing adverse events.
Moderated by: A. Lenore Ackerman, MD, Cedars-Sinai Medical Center, Los Angeles, California
Panelists:
Toby C. Chai, MD, Yale University School of Medicine, New Haven, Connecticut
Duane R. Hickling, MD, The Ottawa Hospital, The Ottawa Research Institute
Kimberly Sue Kenton, MD, MS, Northwestern University, Evanston, Illinois
Ann E. Stapleton, MD, University of Washington, Seattle, Washington
Jennifer T. Anger, MD, MPH, Cedars-Sinai Medical Center, Los Angeles, California
Written by: Hanna Stambakio, BS, Clinical Research Coordinator, Division of Urology, University of Pennsylvania @AStambakio at American Urological Association's 2019 Annual Meeting (AUA 2019), May 3 – 6, 2019 in Chicago, Illinois


