Dr. Ghoreifi and team retrospectively analyzed 247 patients who underwent robotic partial or radical nephrectomy for renal cancer at USC between January 2011 and April 2017. All patients without a 6-month pre-operative Abdomen/Pelvis CT or with any abdominal surgery within 1 year prior to their procedure or with any previous mesh repair were excluded. All CTs, pre- and post-operative, were reviewed to determine the presence of muscle defects and hernias, with any with muscle defects or hernias also excluded. Of the remaining patients, the total psoas area was measured using the right + left psoas areas at the level of L4. Patient were classified as sarcopenic or having decreased skeletal muscle mass if their total psoas area was within the lowest, gender-based tertile. Each muscle defect was identified as either a full muscle defect or a partial muscle defect, while hernias were indexed based on the Tonouchi classification of early, late, or bowel containing.
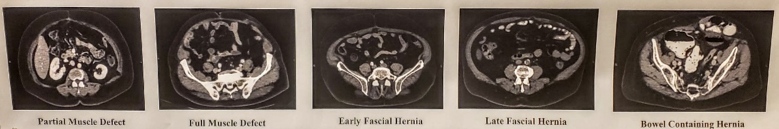
Median follow up time was 2.6 years and the median post-op CT was 4 months postoperatively. The incidence of radiologic trocar site hernias was 27.53% while clinically found hernias had a 3.24% incidence rate. Radiologic and clinical trocar site hernias postoperatively full developed after 1.7 years and 2.6 years, respectively. Evaluation of the radiologically-identified trocar site hernias showed that 10.9% were early fascial hernias, 16.6% were late fascial hernias, and 2.4% were bowel containing hernias. It was noted that all bowel containing hernias were symptomatic and were subsequently surgically repaired. The incidence of both partial and full muscle defects was also found; with partial muscle, defects developing in 14.6% of patients and full muscle defects in 6.5% of patients. Of note, only one patient with an early full muscle defect later had it develop into a hernia. Multivariate analysis demonstrated that of all the variables analyzed, adjuvant therapy, such as chemotherapy or immunotherapy, was the best indicator of trocar site hernia development, with 7 of 12 patients who underwent adjuvant therapy found to have post-treatment trocar site hernias. Additionally, they also found a trend (p=0.07) for the formation of trocar site hernias in patients with a prior abdominal surgery without the use of mesh and which was completed greater than 1 year prior to the radical/partial nephrectomy.
In conclusion, trocar site hernias develop much more frequently than previously believed, though only 11.7% of radiologic hernias become clinically symptomatic. Adjuvant therapy such as chemotherapy, immunotherapy, etc. was the only statistically significant variable associated with trocar site hernia formation, with 58% of the patients who underwent adjuvant therapy later developing trocar site hernias.
Presented by Alireza Ghoreifi, MD, Research Fellow, University of Southern California
Co-Authors: Authors: Alireza Ghoreifi*, Gilbert Whang, Mohammad Aslzare, Madeleine Burg, Benjamin Liu, Xiaomeng Lei, Khoa Tran, Tapas Tejura, Vinay Duddalwar, Mihir Desai, Monish Aron, Inderbir Gill, and Hooman Djaladat
Affiliation: The University of Southern California, Keck School of Medicine, Los Angeles, CA
Written by: Vinay Cooper, (Department of Urology, University of California-Irvine) at the American Urological Association's 2019 Annual Meeting (AUA 2019), May 3 – 6, 2019 in Chicago, Illinois


