Dr. Winter and team found and analyzed the 83 patients who underwent open or robotic level II/III IVC tumor thrombectomy between November 2007 and December 2017. After 3D reconstructions were obtained using the Synapse system, a single experienced uro-radiologist quantified the tumor, renal vein, and IVC volumes of the preoperative CT/MRIs. These were then compared to surgical outcomes including operative time, transfusion rate, EBL, length of stay, and complications. They then performed both univariate and multivariable regression analysis to find any independent associations between the surgical outcomes, demographic, and volumetric data. Total tumor volume was calculated as the renal tumor volume + renal vein thrombus volume – IVC thrombus volume.
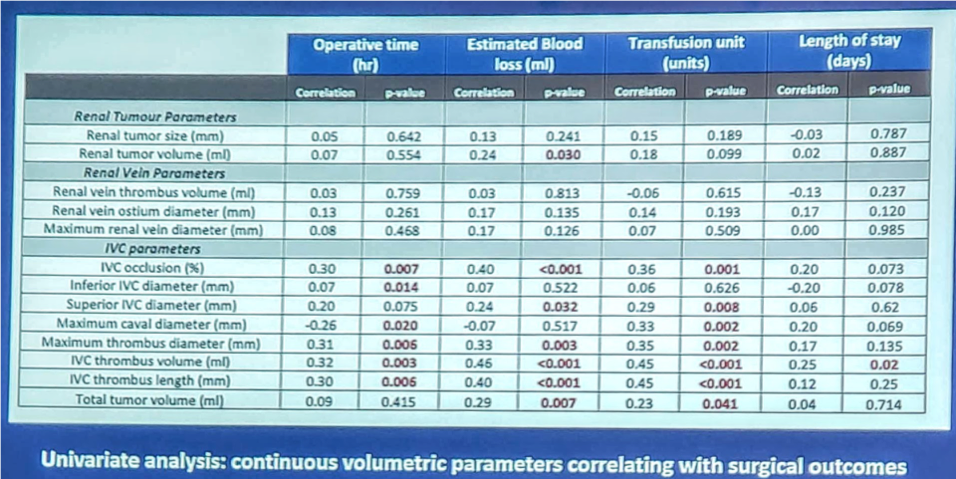
There were 56 total complications, 42% of which were Clavien grade I/II and a total of 5 deaths, a mortality rate of 6%. Univariate analysis of the demographic factors compared to the surgical outcomes showed that patients <61 years old, had a BMI >27, ASA ≥ 3, or who underwent and open IVC thrombectomy had a statistically significant higher EBL. Volumetric parameters versus the surgical outcomes demonstrated that almost all the IVC measurements were significant with increased operative time, increased EBL, and increased number of transfusion units. As the IVC thrombus volume was the most significant of the comparisons, it was run through multivariate linear regression. This showed IVC thrombus volume to be an independent predictor of operative time, EBL, need for transfusion, length of stay, and overall complication rate. Further calculations derived that, for each 10mL of IVC thrombus volume increase, there was a 12 minute increase in operative time, a 64mL increase in EBL, 0.8 unit increase in transfusion, andd a 0.9 day increase in the length of stay. Variations of the thrombus volume, <23mLs and ≥23mLs, were then compared to the surgical outcomes, showing that if the thrombus volume was ≥23mLs, then the patients had statistically increased operative time, EBL, and transfusion unit amount. There was no difference between Mayo level II and Mayo level III thrombi.
In conclusion, 3D reconstruction and subsequently calculated tumor volumetrics including the IVC thrombus volume can be used to predict surgical outcomes in level II and III caval thrombectomy. The presenter was questioned whether his group was using the studied volumetric data to determine the surgical approach, to which Dr. Winter noted that currently, they are not using it to determine the surgical approach, though may look into that into the future.
Presented by: Matthew Winter, MD, University of Southern California, Keck School of Medicine, Los Angeles, CA
Written by Vinay Cooper, Department of Urology, University of California-Irvine, at American Urological Association's 2019 Annual Meeting (AUA 2019), May 3 – 6, 2019 in Chicago, Illinois
Authors: Matthew Winter*, Alessandro Tafuri, Rivas Marielena, Giovanni Cacciamani, Shane Pearce, Aliasger Shakir, Luis Medina, Akbar Ashrafi, Walter Artibani, Andre Abreu, Monish Aron, Mihir Desai, Djaladat Hooman, Anne Schuckman, Sia Daneshmand, Vinay Duddalwar, and Inderbir Gill


