The objective of this study was to assess the cancer detection rate and comprehensive post-biopsy outcomes of a modified 12-core transperineal template mapping biopsy. The authors reviewed the Michigan Urologic Surgery Improvement Collaborative (MUSIC) prospective registry and searched for all patients undergoing transperineal or transrectal prostate biopsy at a single pilot MUSIC site between 3/2017 and 12/2018. Transperineal prostate biopsy was performed under local anesthesia using the PrecisionPointTM device to complete a modified Barzell 12-core biopsy (figure 1).
Figure 1 – Barzell 12-core prostate biopsy:

For this study, all relevant patient characteristics, cancer detection rates, and 30-day complication rates were prospectively collected and analyzed. Multivariable analysis was performed to control for relevant risk factors. Only biopsy-naïve men were included in the cancer detection rate analysis. High-grade cancer was defined as a Gleason score of 7 or above. The study flow diagram is shown in Figure 2.
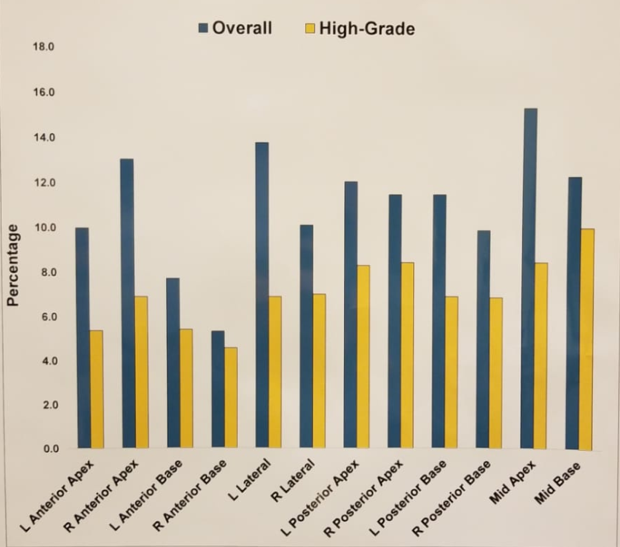
A total of 189 transperineal and 1284 transrectal prostate biopsies were performed. The overall cancer detection rate was 43.4% (82/189) for transperineal biopsies compared to 57.5% (738/1284) for transrectal biopsies (p < 0.001). The cancer detection rate of high-grade cancers was 22.2% (42/189) for transperineal biopsies and 35.1% (451/1284) for transrectal biopsies (p<0.001). The overall and high-grade detection based on transperineal core location is shown in Figure 3.
Figure 2: Study flow diagram:

Figure 3: Overall and high-grade detection rate based on transperineal core location:
In the multivariable model, after adjusting for relevant covariates, transperineal biopsies were associated with significantly lower odds of cancer detection rates (OR=0.56, 95% CI 0.41-0.78, p<0.01), and high-grade cancer detection rate (OR=0.57, 95% CI 0.38-0.84, p<0.01) as shown in table 1. Other factors that were associated with an increased cancer detection rate of all cancers included PSA, age, abnormal digital rectal examination, and positive family history. For high-grade cancer detection rates, the same covariates were shown to increase the risk except for positive family history.
Table 1: Factors associated with overall and high-grade detection rate:

Following transperineal biopsies, there were no hospitalizations due to infections (including urinary tract infections), sepsis episodes, fever, or acute urinary retention (Table 2). In contrast, infectious complications did occur following transrectal biopsies (3.5% in total).
Table 2: Rate of post-biopsy complication rates:

The authors concluded that transperineal biopsies were associated with a decreased overall and high-grade cancer detection rate, compared to transrectal biopsies. Early outcomes of transperineal biopsies demonstrated zero infectious complications within 30 days. Lastly, the right and left anterior-base cores demonstrated the lowest cancer detection rate.
Presented by: Adam Cole, MD, Michigan Urological Surgery Improvement Collaborative, Ann Arbor, Michigan, United States
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the American Urological Association's 2019 Annual Meeting (AUA 2019), May 3 – 6, 2019 in Chicago, Illinois


