The evolution of focal therapy resulted from the over diagnosis and over the treatment of prostate cancer considering that all therapies have side effects, primarily sexual and urinary in nature. The solution is an outpatient/same day treatment that lowers the sexual/urinary side effects (without a long-term catheter). However, the evidence for durable cancer control is what we currently lack. Currently, the majority of low risk cases are treated radically. 50-75% of men with low risk cancer choose active surveillance upfront (including 50% in MUSIC and 75% in CAPSURE), however 25-60% cross-over to radical treatment in ~5-10 years.
In a study assessing histological characteristics of the index lesion in 100 patients, the role of prostate cancer focality in selecting men for focal therapy was evaluated [1]. Cases that would have been suitable for focal ablation were also evaluated. Tumors were more often multifocal (78%) and bilateral (86%) – 270 tumor foci were identified. In multifocal disease, tumour volume, Gleason score and pathological stage were almost invariably defined by the index lesion of the specimen and using the defined criteria, 51% of men in this series would have been considered suitable for focal ablation of the index lesion.
A 2015 consensus meeting on focal therapy identified inclusion criteria of PSA <20 ng/mL, T1c-T2a, up to Gleason 7 disease (ie. intermediate risk), a life expectancy of >10 years and any prostate volume. Dr. Rastinehad notes that the best way to implement focal therapy is to perform pre-biopsy mpMRI followed by targeted biopsies of visible lesions. This has/will lead to a paradigm shift to the detection of higher grade disease and visualization of prostate cancer. He notes that prostate is the last solid organ malignancy that imaging did not play a role in the diagnosis.

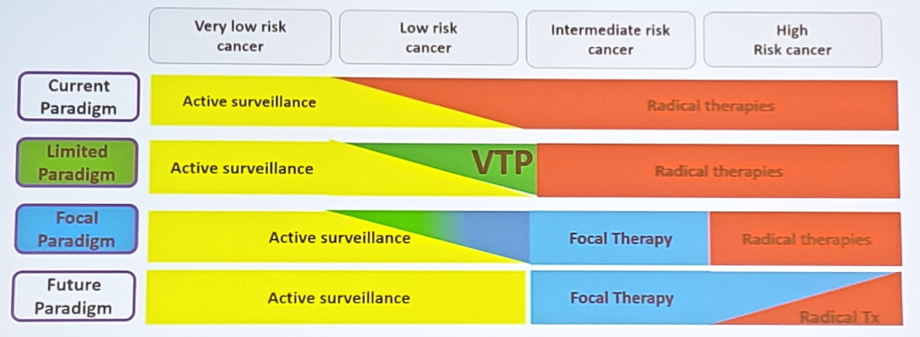
The current recommendations for following patients post-therapy are somewhat ambiguous but generally include PSA and imaging as triggers – generally it is agreed that patients should have an evaluation by at least 1 year to assess the efficacy of the intervention. So, how does focal therapy fit into the paradigm of treatment? Currently it is not specifically in the paradigm, however, Dr. Rastinehad thinks that a future paradigm will include active surveillance followed by several indications for focal therapy – radical treatment only used in a handful of patients.
Dr. Rastinehad concluded with several take home messages:
Presented by: Art Rastinehad, Icahn School of Medicine at Mount Sinai, New York, New York
Written By: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University - Medical College of Georgia, Twitter: @zklaassen_md at the American Urological Association's 2019 Annual Meeting (AUA 2019), May 3 – 6, 2019 in Chicago, Illinois
References:
- Patients eligible for focal therapy should have biopsy-confirmed imaging visible lesions with clinically significant prostate cancer defined as any GGG >= 2 and may be used as a target for focal therapy
- Biomarkers and MR imaging should be used with targeted biopsy in conjunction with the standard biopsy when evaluating patients
- Patients should have a biopsy to confirm ablation by ~1 year post-treatment
Presented by: Art Rastinehad, Icahn School of Medicine at Mount Sinai, New York, New York
Written By: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University - Medical College of Georgia, Twitter: @zklaassen_md at the American Urological Association's 2019 Annual Meeting (AUA 2019), May 3 – 6, 2019 in Chicago, Illinois
References:
- Karavitakis M, Winkler M, Abel P, et al. Histological characteristics of the index lesion in whole-mount radical prostatectomy specimens: Implications for focal therapy. Prostate Cancer Prostatic Dis 2011 Mar;14(1):46-52.


