Dr. Davies notes that the FDA Commissioner recently stated: “Until clinicians stop prescribing opioids far in excess of clinical need, this crisis will continue unabated.” Indeed, 75% of abused opioids come/stolen from MDs, their friends or relatives. Dr. Davies notes that there have been three waves in the rise in opioid overdose deaths:
- Wave 1 (starting in 1999): rise in prescription opioid overdose deaths (ie. natural and semi-synthetic opioids and methadone)
- Wave 2 (starting in 2010) rise in heroin overdose deaths
- Wave 3 (starting in 2013) rise in synthetic opioid overdose deaths (ie. tramadol and fentanyl)

This is a composite of multiple distinctive subepidemics of different drugs (primarily prescription opioids, heroin, methadone, synthetic opioids, cocaine, and methamphetamine), each with its own specific demographic and geographic characteristics.
Furthermore, Dr. Davies notes that there is new persistent opioid use among opioid naïve patients after undergoing elective procedures:
- Hepatobiliary: 6%
- Knee/hip surgery: 8%
- Hand surgery: 13%
- Spine surgery: 13%
- Pediatric surgery: 5%
- Elective oncology: 10%
- Decrease opioids in our community
- Decrease persistent opioid use in our patients
- Decrease massive overprescribing
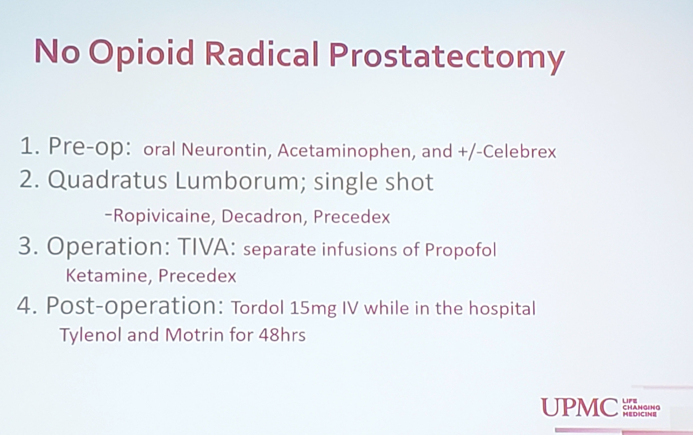
Following the implementation of this protocol and a number of “nudges” to his faculty via lectures, guidelines, texts, and emails, Dr. Davies notes that average number of pills prescribed after radical prostatectomy went from 40 prior to implementation down to 2 in February 2019. Furthermore, when evaluating patients with pain/satisfaction surveys, patients were not suffering in pain from the lack of opioids.
Dr. Davies concluded with several take homes messages/”warning facts”:
- More people died of opioid overdose than prostate cancer last year
- Persistent opioid use is the #1 “surgical complication”
- >95% of men require no opioid use for their radical prostatectomy and they should not be ordered routinely
Presented by: Benjamin Davies, Professor at the University of Pittsburgh School of Medicine, Chief of the Urology Section at the Shadyside/Hillman Cancer Center, Director of the Urologic Oncology Program, Pittsburgh, PA
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University - Medical College of Georgia, Twitter: @zklaassen_md at the American Urological Association's 2019 Annual Meeting (AUA 2019), May 3 – 6, 2019 in Chicago, Illinois
References:
- Jalal H, Buchanich JM, Roberts MS, et al. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science. 2018 Sep 21;361(6408).


