The surgical experience may be a patient’s first exposure to opioids. For some patients, that exposure can ultimately lead to opioid abuse and misuse. Anesthesiologists have the unique expertise to develop and utilize pain control alternatives that can reduce patient exposure to and use of opioids during surgery and at discharge.
There are several opioid sparing techniques that can be performed for surgical pain. The first is regional anesthesia – local anesthetics can be used to numb the surgical part of the body which is being operated on. The other technique is a multimodal approach – in which pain is being treated with different combinations of drugs targeting different pain pathways. Multiple randomized controlled trials have demonstrated a decrease in immediate acute pain scores and reduced opioids with this technique. A meta-analysis assessing the use of transversus abdominis plane (TAP) blocks for laparoscopic procedures demonstrated reduced opioid requirements postoperatively.
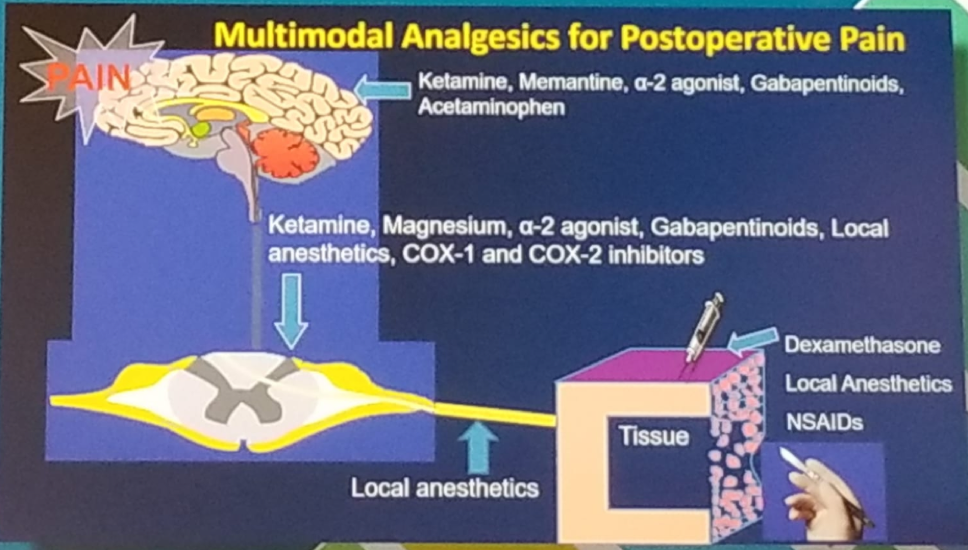
Multimodal analgesia is the combination of different analgesics that act by different mechanisms resulting in additive or synergistic analgesia with lowered adverse effects; compared to sole administration of an individual pharmacological agent. The goal is to decrease the use of postoperative opioids. Figure 1 demonstrates the main principles used and the medications that can be given for multimodal analgesia.
Commonly used non-opioid analgesics include:
- Lidocaine and Ketamine
- Anticonvulsants -gabapentin and pregabalin
- Acetaminophen
- Non-steroidal anti-inflammatory drugs – including non-selective and selective cyclooxygenase inhibitors
Figure 1 – Multimodal analgesia:
Next, Dr. Buvanendran moved on to discuss the many risk factors for postoperative chronic opioid use. These include preoperative opioid use (which represents a potentially modifiable risk factor and a novel target to improve quality and value of surgical care), preoperative benzodiazepines and antidepressants, preoperative pain, history of drug, alcohol, or tobacco abuse, lower socioeconomic status, and medical comorbidities (pulmonary disease, heart failure, and depression). The Center for Disease Control (CDC) has issued opioid guidelines for primary care physicians. These guidelines provide recommendations for the prescribing of opioid pain medication by primary care clinicians. These recommendations are for chronic pain in outpatient settings, outside of active cancer treatment, palliative care, and end-of-life care. The guidelines are intended to ensure that clinicians and patients consider safer and more effective treatments. Finally, the recommendations in the guidelines are voluntary, rather than prescriptive standards. They are based on emerging evidence, including observational studies or randomized clinical trials, with notable limitations. Clinicians should consider the circumstances and unique needs of each patient when providing care. According to these guidelines, long-term opioid use often begins with the treatment of acute pain. When opioids are used for acute pain, providers should prescribe the lowest effective dose of immediate-release opioids. They should prescribe no greater quantity than needed for the expected duration of pain severe enough to require opioids.
The CDC is trying to raise awareness of the following issues that could put patients at risk:
- Misapplication of recommendations to populations outside of the guideline’s scope.
- Misapplication of the guideline’s dosage recommendation that results in hard limits or “cutting off” opioids.
- The guideline does not support abrupt tapering or sudden discontinuation of opioids.
In conclusion, the size and scope of the US opioid epidemic require immediate sweeping action from Federal and local governments, health care professionals and drug companies. Every health care provider must be aware of multimodal analgesia for postoperative pain, making it routine care for patients, with a final goal of reducing opioid prescriptions.
Presented by: Asokumar Buvanendran, MD, Vice Chair of Research, Director of Orthopedic Anesthesia, Rush University Medical Center, Chicago, Illinois
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, Twitter: @GoldbergHanan at the American Urological Association's 2019 Annual Meeting (AUA 2019), May 3 – 6, 2019 in Chicago, Illinois


