The authors first identified 2034 patients who underwent partial or radical nephrectomy at their institution between 2012 and 2014. They then identified tumors with one of more of the following aggressive pathological features: RCC ≥pT3a, grade 4, sarcomatoid/rhabdoid component, or unclassified subtype; collecting duct or renal medullary carcinoma; invasive urothelial carcinoma; malignancies other that RCC or urothelial carcinoma; pathologic nodal involvement. In total, 580 patients from their institutional database had a surgical resection specimen which demonstrated locally advanced or otherwise aggressive histology. Of these, 39 patients did not have adequate pre-operative imaging for assessment. Thus, the authors examined 541 patients with pathologic evidence of locally advanced or otherwise aggressive histology and adequate preoperative imaging.
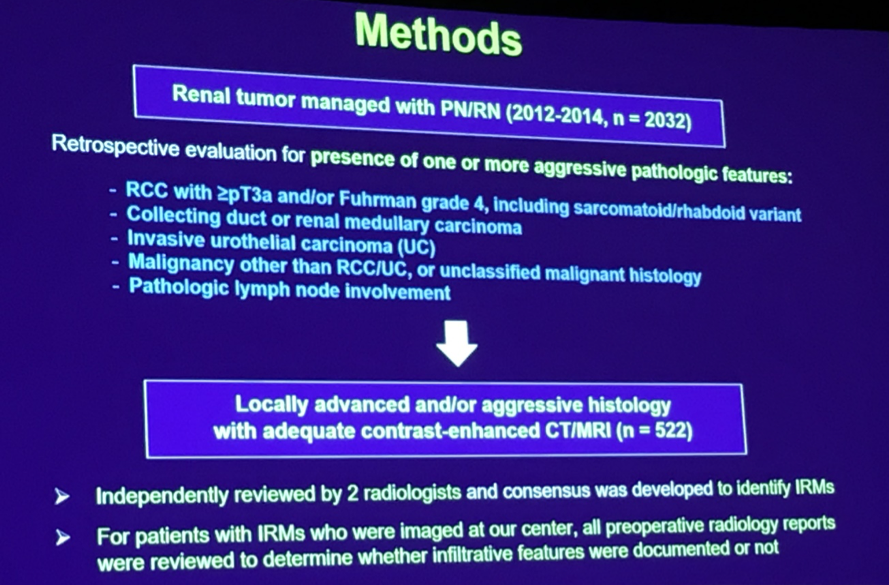
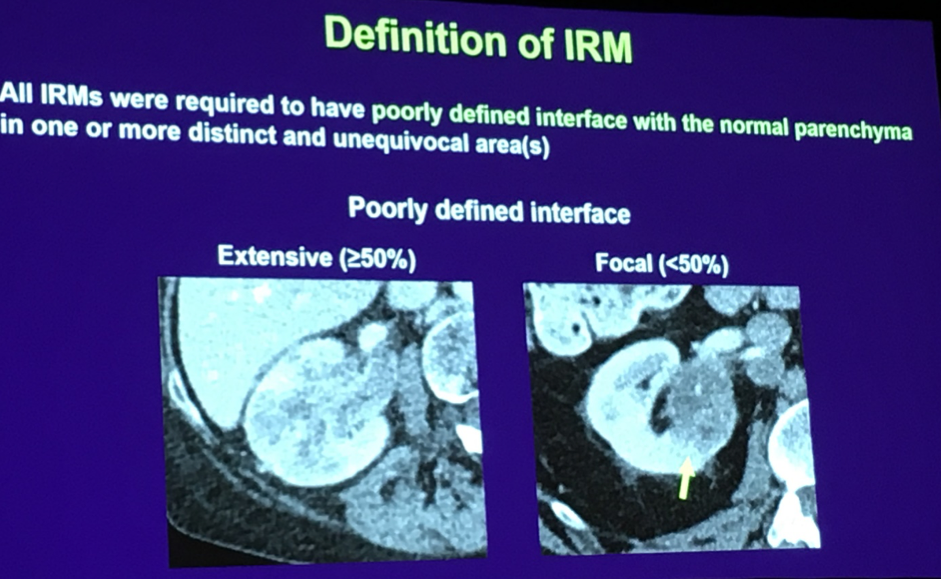
The authors then examined the patients’ preoperative imaging in an attempt to ascertain if infiltrative features could be identified preoperatively. Imaging was deemed consistent with infiltrative disease where there was a poorly defined contour and markedly irregular shape to the tumor.
Of these 541 patients, 409 (76%) demonstrated no features of infiltrative disease on preoperative imaging. 132 patients had preoperative evidence of infiltrative renal masses based on preoperative imaging. Of these, pathologic analysis demonstrated 102 to be renal cell carcinoma and 22 to be urothelial carcinoma. Of the RCCs, 39 demonstrated sarcomatoid or rhabdoid features, a further 21 were grade 4, and 18 were unclassified. The median tumor size exceeded 8cm and most (92%) were considered high complexity according to R.E.N.A.L. scoring. The majority of these patients (77%) were symptomatic and 50 (38%) presented with disseminated disease.
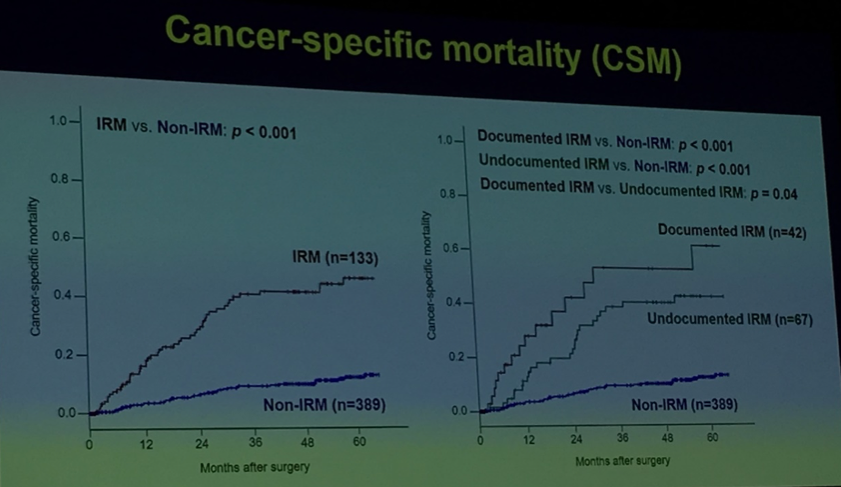
The majority (104/132) underwent preoperative imaging at the same institution as their surgery. Of these, only 40 (38%) were identified as infiltrative renal masses on the basis of radiologic interpretation and only a further 4 (4%) were identified as infiltrative by the surgical team. Thus, the majority of tumors (60/104) were no documented as infiltrative prior to pathological analysis. In patients where infiltrative tumors were not identified preoperatively, poorly defined contours and irregular shape were more likely to be focal (rather than extensive), compared with those where this was identified preoperatively.
Despite a relatively limited median follow-up of 25 months, 63% of the patients experienced recurrence and 44% died. There were no differences in recurrence or survival based on preoperative identification of infiltrative disease (p=0.60). However, time to death was shorter among patients with preoperatively identified infiltrative disease (12 months) as compared to those for whom it was not preoperatively identified (25 months; p=0.02), suggesting a poor prognosis for those patients where these features are sufficiently advanced to be radiologically apparent.
Presented by: Hajime Tanaka, MD, Ph.D, Nagoya City University, Nagoya
Co-authors: Xiaobo Ding, Yanbo Wang, Yunlin Ye, Rebecca A. Campbell, Molly E. Dewitt-Foy, Chalairat Suk-Ouichai, Ryan D. Ward, Erick M. Remer, Steven C. Campbell
Written by: Christopher J.D. Wallis, Urology Resident, University of Toronto, @WallisCJD on Twitter at the American Urological Association's 2019 Annual Meeting (AUA 2019), May 3 – 6, 2019 in Chicago, Illinois


