(UroToday.com) In a plenary session at the American Urologic Association Virtual Annual Meeting, Dr. Seth Lerner moderated a session designed to answer the question of “What to do During BCG Shortage for High-Risk NMIBC Patients?.” Along with panelists Drs. Steve Boorjian, Ashish Kamat, James McKiernan, Chad Ritch, and Dr. Lerner explored a number of treatment options.
To begin, Dr. Lerner provided context, highlighting the current status of the Bacille Calmette-Guérin (BCG) shortage as well as risk stratification and guideline recommendations. With respect to the BCG shortage, Dr. Lerner reviewed the situation highlighting that the Connaught strain (produced by Sanofi Pasteur) has been off-line since 2012 with confirmed permanent closure as of 2017. As a result, the sole source is the Merck manufactured Tice strain which is produced in a single plant for distribution to 70 countries.
As a result of BCG shortages, a number of recommendations were made as part of a joint statement from the AUA, AACU, BCAN, SUO, LUGPA, SUO, and UCF. First, the joint statement highlighted that BCG should not be used for patients with low-risk disease. In patients with intermediate-risk disease, intravesical chemotherapy should be used as a first-line treatment with an alternative chemotherapeutic agent used as second-line therapy. Patients with high-risk non-muscle invasive bladder cancer should be prioritized to receive BCG which full-strength treatment courses recommended. Where this is not possible, dose reduction to ½ or 1/3 dose was recommended. Where there is sufficient supply for maintenance therapy, the joint statement recommended the use of a 1/3 dose with a one year course. Further, limited BCG supplies should be prioritized for induction therapy among BCG-naïve patients with high-risk disease and maintenance therapy should be de-prioritized. Where BCG is not available, chemotherapeutic options included mitomycin, gemcitabine, epirubicin, docetaxel, valrubicin, or sequential treatments with gemcitabine/docetaxel or gemcitabine/mitomycin.
Based on personal communication, Dr. Lerner conveyed that Merck considers the production of BCG at maximal capacity to be a priority. In the meantime, he highlighted that BCG dose reduction may actually provide benefit as an appropriate cytokine response may be observed with very low disease, as little as 1/100th of a standard treatment dose. Further, the AUA split dosing policy supports the use of the same vial for more than one patient to avoid wastage.
Dr. Kamat then discussed how to prioritize the utilization of limited BCG supplies. He highlighted the IBCG risk stratification approach for patients with intermediate-risk disease.
In somewhat of a contrast from Dr. Lerner, Dr. Kamat highlighted that the optimal maintenance approach is the SWOG/”Lamm” protocol with 6+3 approach which shows a significant benefit.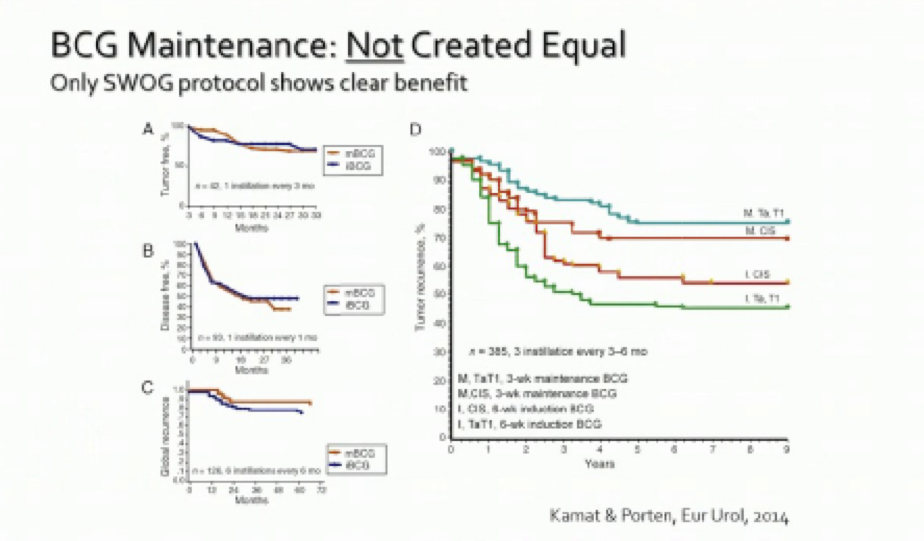
In addition, he highlighted that the duration of therapy (1 versus 3 years) appears to be more influential than dosage (1/3 versus full dose) as highlighted in data from the EORTC 30962 trial: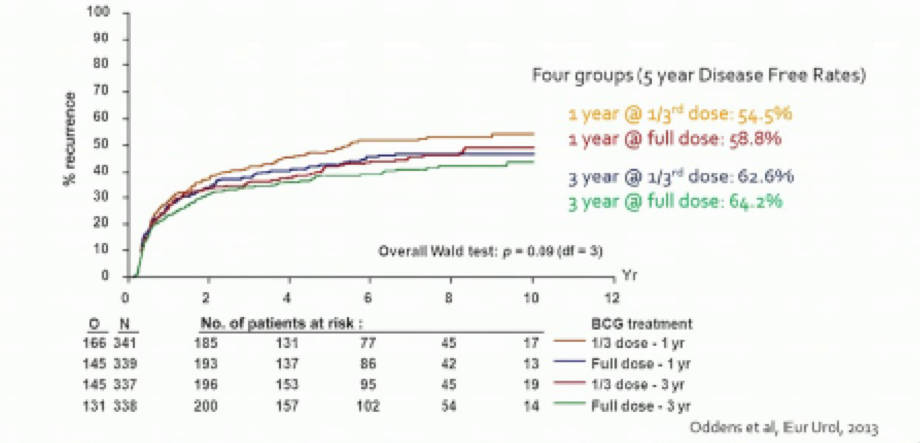
In keeping with the guideline recommendations highlighted by Dr. Lerner, Dr. Kamat offered a summary of the recommendations for prioritizing the use of limited BCG resources including induction in high-risk patients and maintenance according to the SWOG protocol.
As discussed above, the EORTC 30962 trial showed no difference between 1/3 dose and full-dose BCG in patients with high-risk disease. Dr. Ritch then discussed practical approaches to applying this in clinical practice.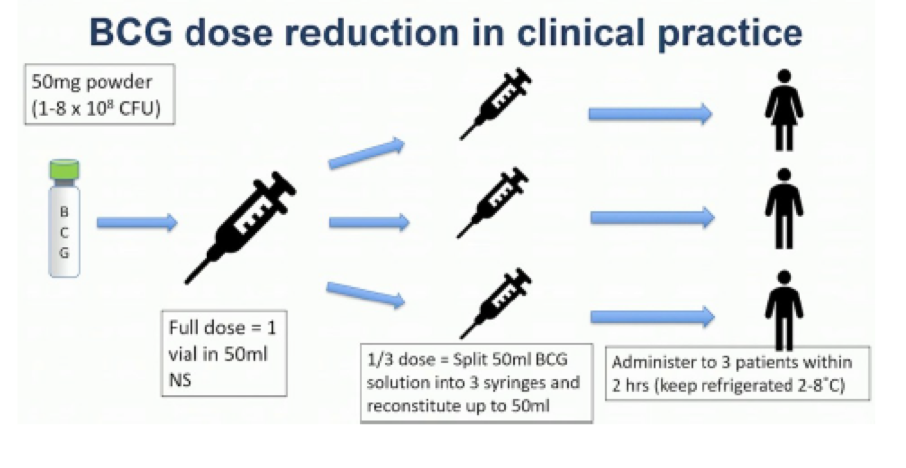
In addition, he highlighted that, in July 2019, the HCPCS billing code J9030 allowed for billing for multiple uses of a single vial of BCG. He also highlighted alternatives to BCG including intravesical chemotherapy with mitomycin C, valrubicin, gemcitabine, and nab-paclitaxel. MMC is the most readily available option and Dr. Ritch discussed approaches to optimize MMC.
Dr. McKiernen then discussed a variety of novel chemotherapeutic regimes including single-agent valrubicin, gemcitabine, taxanes, and electromotive or hyperthermic mitomycin and multi-agent regimes.
In the single-agent space, meta-analysis has assessed gemcitabine versus BCG in NMIBC without differences in recurrence, progression, or toxicity.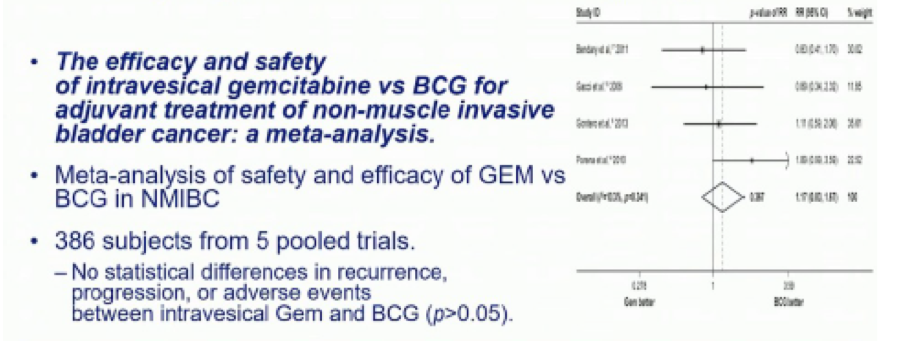
In patients with prior BCG failure, treatment with gemcitabine was associated with better recurrence free survival than re-induction with BCG.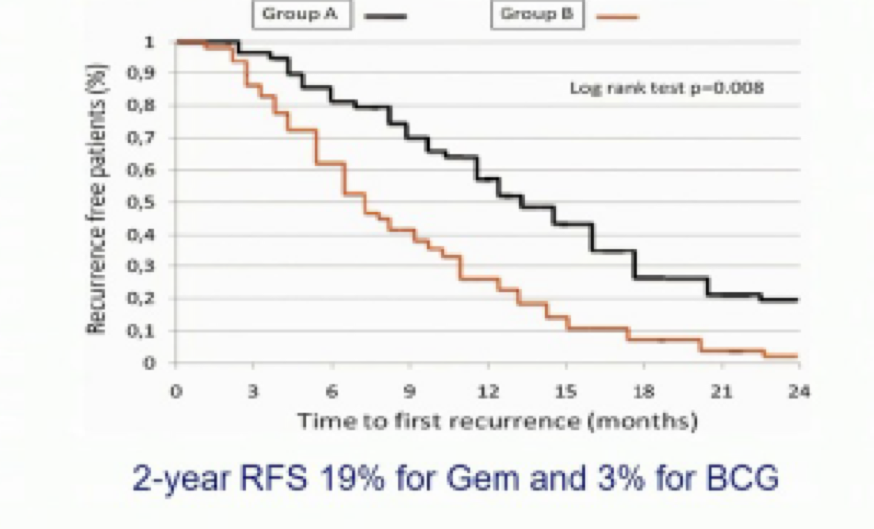
Dr. McKiernan then discussed combination regimes starting with gemcitabine plus docetaxel. This has typically been used in patients who are BCG unresponsive disease. More recently, a combination of cabazitaxel, gemcitabine, and cisplatin has been explored. In data published in March 2020, this approach demonstrated promising results.
Dr. Boorjian then presented on the treatment of patients with BCG unresponsive disease. He highlighted than the key concept was to avoid further use of BCG, particularly in the setting of a BCG shortage where we don’t want to waste BCG on patients who are unlikely to benefit. He highlighted that the AUA/SUO guidelines recommend offering radical cystectomy in patients with high-risk disease who have recurrent or persistence following two induction cycles of BCG. For those in whom cystectomy in unsuitable or refused, the guidelines suggest clinical trials with the use of intravesical chemotherapy when/where clinical trials are unavailable.
He noted that pembrolizumab was recently FDA approved for patients with BCG unresponsive CIS +/- papillary tumors on the basis of benefits demonstrated in the single-armed phase II KEYNOTE-057 trial. He then postulated what the future may hold including a number of agents currently under investigation.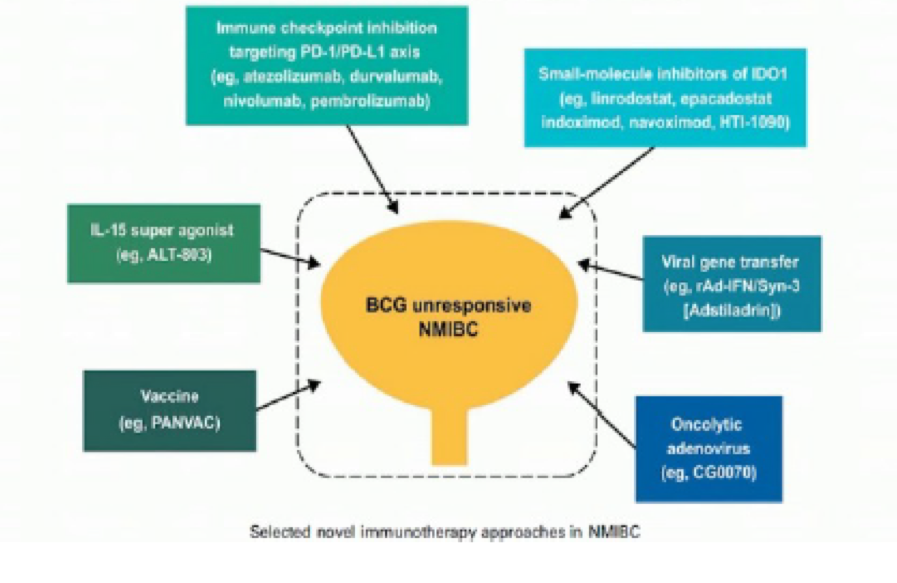
The panelists highlighted data showing that the BCG shortage has resulted in increased rates of recurrence and increased utilization of cystectomy, even within risk groups.
In closing, they offered a few recommendations in the scenario of no available BCG including a risk-stratified approach utilizing chemotherapy, combination chemotherapy, and radical cystectomy on the basis of risk of progression and recurrence.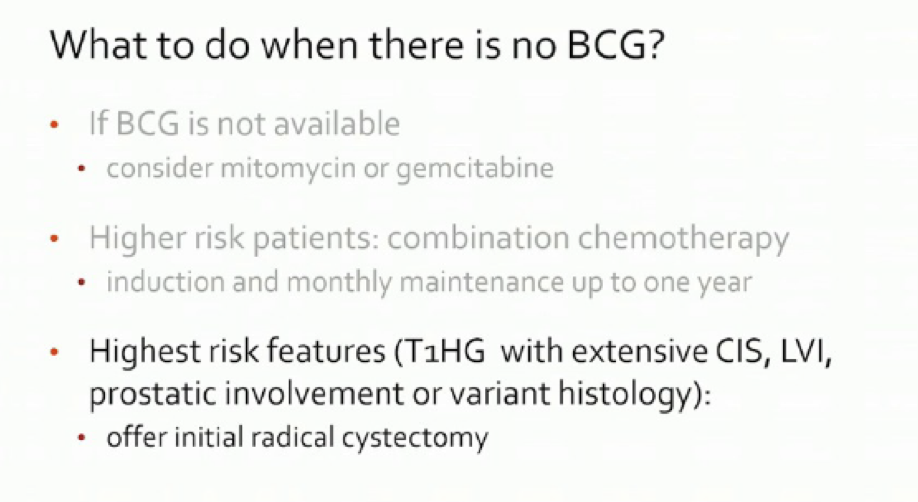
Presented by: Seth P. Lerner, MD, FACS, Vice Chair for Faculty Affairs, Baylor College of Medicine, Houston, TX
Written by: Christopher J.D. Wallis, MD, PhD, Urologic Oncology Fellow, Vanderbilt University Medical Center Contact: @WallisCJD on Twitter at the 2020 American Urological Association (AUA) Annual Meeting, Virtual Experience #AUA20, June 27- 28, 2020
Related Content:
Read: ASCO GU 2020: Management Strategies in the Face of the Bacillus Calmette-Guérin Shortage


