The RAZOR trial was a multicenter, open-label non-inferiority phase III randomized trial comparing robotic-assisted radical cystectomy (RARC) to open cystectomy (OC). In this analysis, the authors used the per-protocol population of the RAZOR trial. Complications up to 90 days postoperatively were graded using the Clavien-Dindo system. Baseline characteristics were captured including frailty as evaluated by the validated simplified frailty index (sFI) (ECOG≥2, history of diabetes mellitus, chronic obstructive pulmonary disease, congestive cardiac failure, and hypertension requiring treatment). Multivariable logistic regression analysis was conducted to identify factors predicting major complications (Clavien-Dindo grade 3 and above) up to 90 days following surgery.
The authors found no significant difference in overall and major complication rates between RARC and OC. Gastrointestinal (predominantly ileus) and urinary tract infections were the most common complications in both groups. Female sex (OR 1.84, 1.08-3.16, p=0.026) and frailty (sFI ³3) (OR 5.90, 2.65-13.14, p<0.0001) were significant predictors of major complications at 90 days postoperatively. Surgical approach (RARC or OC), diversion type, chemotherapy, lymphadenectomy extent, age, T or N stage, and BMI were not predictive (Table).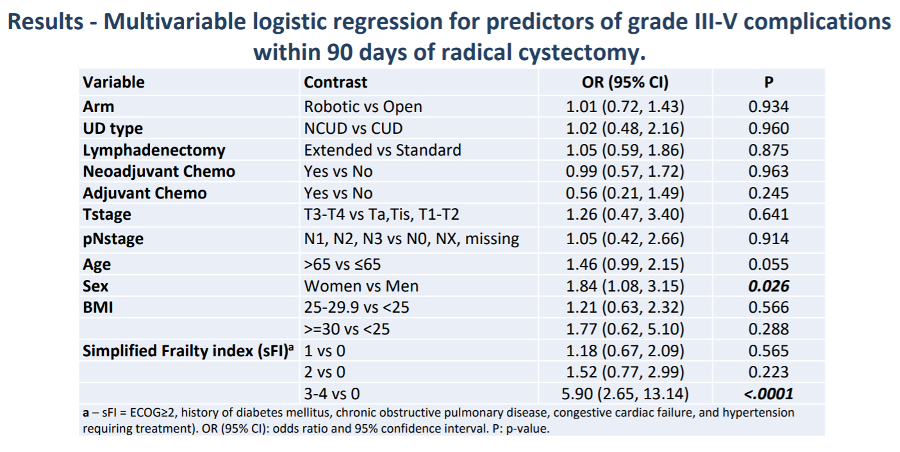
Despite hope based on non-randomized data, analysis of the largest RCT to date demonstrates that postoperative complication rates do not differ between RARC and ORC in this analysis from the RAZOR trial. These data suggest that inherent patient factors, rather than surgical technical factors, drive postoperative complications following cystectomy.
Presented by: Vivek Venkatramani, MD, University of Miami Miller School of Medicine, Miami, FL
Co-Authors: Isildinha M Reis, Nachiketh Soodana-Prakash, Maria F Becerra, Mark L Gonzalgo, Erik P, Micheal E Woods, Robert S Svatek, Alon Z Weizer, Ann Harbour, MI, Badrinath R Konety,, MN Minneapolis, Mathew Tollefson, Tracey L Krupski, Norm D Smith, Ahmad Shabsigh, Daniel L Barocas, Marcus L Quek, Atreya Dash, and Dipen J Parek
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, @WallisCJD on Twitter at the 2020 American Urological Association (AUA) Annual Meeting, Virtual Experience #AUA20, June 27- 28, 2020
Related Content:
Read: Predictors of Recurrence, Progression-Free and Overall Survival Following Open Versus Robotic Radical Cystectomy: Analysis from the RAZOR Trial with a 3-Year Follow-Up.


