The authors identified 3,468 patients diagnosed with a cT1-2 cN0 cM0 renal mass who underwent RAPN or OPN at 9 high-volume European, North American, or Asian Institutions. These individuals were prospectively identified, and outcomes were collected in a central database. For the purposes of this analysis, the authors examined perioperative complications, renal function, and cancer control. Regression analysis and propensity-score matching were used to account for all measurable potential confounders with special attention to key determinants of clinical outcomes including tumor complexity and surgical experience.
Rate of complications and peri-operative functional outcomes favored patients undergoing RAPN compared to OPN as shown in the following table. Oncologic outcomes and longer-term survival outcomes were similar between groups.
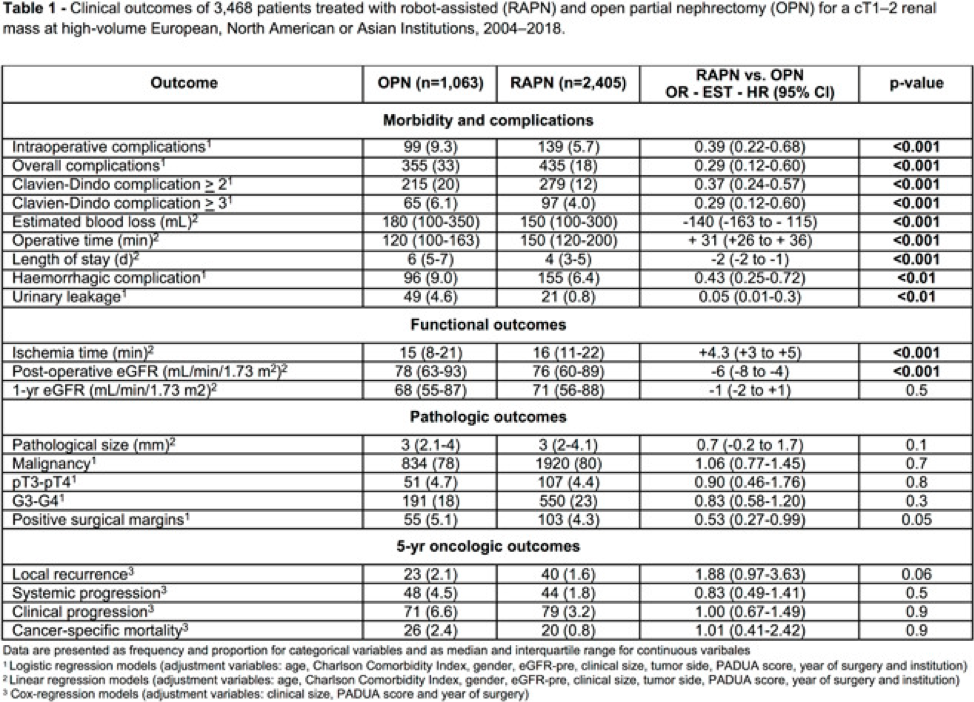
On multivariable analysis accounting for all measurable potential confounders, relative to OPN, RAPN was associated with a lower rate of any intraoperative (5.7 vs 9.3%) or postoperative (18 vs 33%) complications. After stratification according to complication severity or type, relative to OPN, RAPN was associated with a lower rate of Clavien-Dindo ≥2 (12 vs 20%), Clavien-Dindo ≥3 (4 vs 6.1%), hemorrhagic (6.4 vs 9%) and urinary leakage-related (0.8 vs 4.6%) complications.
Conversely, relative to OPN, RAPN was associated with marginally longer ischemia time (16 vs 15 min) and transiently lower postoperative estimated glomerular filtration [eGFR] (76 vs 78 mL/min) but similar 1-year eGFR (71 vs 68 mL/min). No difference was recorded with respect to the rate of positive surgical margins (4.3 vs 5.1%) or local recurrence (1.6 vs 2.1%), systemic progression (1.8 vs 4.5%) and cancer-specific mortality (0.8 vs 2.4%) at a median follow-up of 32 months. These observations were confirmed also after accounting for individual items defining tumor complexity and surgical experience.
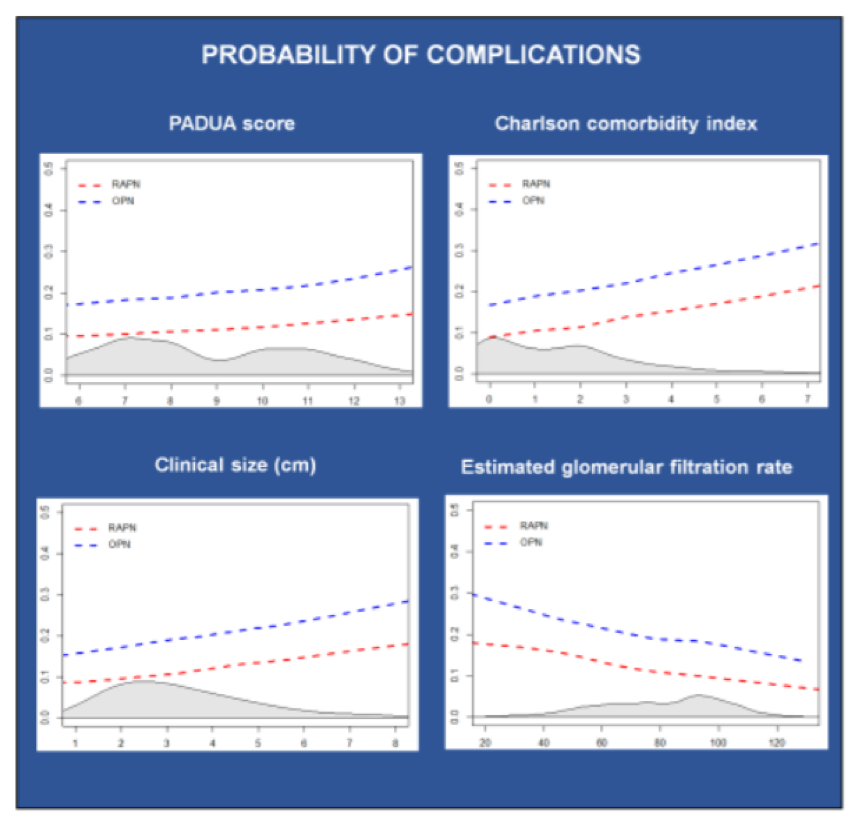
Together, these data demonstrate that RAPN is associated with lower morbidity and similar oncologic and long term renal function outcomes.
Presented by: Alessandro Larcher, MD, Vita Salute San Raffaele University, Milan, Italy
Written by: Christopher J.D. Wallis, MD, PhD, Urologic Oncology Fellow, Vanderbilt University Medical Center, Nashville, TN, Twitter: @WallisCJD, at the 2020 American Urological Association (AUA) Annual Meeting, Virtual Experience #AUA20, June 27- 28, 2020.


