(UroToday.com) Patients who undergo surgical resection of renal cancers are at risk of chronic kidney disease (CKD). The involvement of nephrologists, through nephrology referral for at-risk patients, is recommended per 2017 American Urologic Association guidelines, although adherence and its effects are uncertain. In a podium presentation at the American Urologic Association (AUA) 2020 Virtual Annual Meeting, Julia Wainger, MD, and colleagues examined nephrology referral rates amongst renal cancer nephrectomy patients to assess referral predictors and study associations of nephrology referral and survival.
The authors used data from the SEER-Medicare database to identify patients ≥66 years old who underwent nephrectomies for malignancy between 1999 and 2014 (N=25,641). The authors identified nephrology referrals on the basis of nephrology claims and identified if and when patients were referred by CKD disease status and surgery type. They then used logistic regression to identify associated patient factors and used a Cox proportional hazard regression model to assess associations with survival with logistic regression and survival analyses conducted for cases from 2004-2014 with available comorbidity data (N=16,612).

Among 25,641 patients who underwent nephrectomy between 1999 and 2014, 16.3% had pre-operative CKD and 43.4% of patients developed post-operative CKD. Of those who had post-operative CKD, 4.8% of patients were referred pre-operatively and 50.2% post-operatively to nephrology, with referral rates differing based on CKD status and surgical approach as demonstrated in the following figure: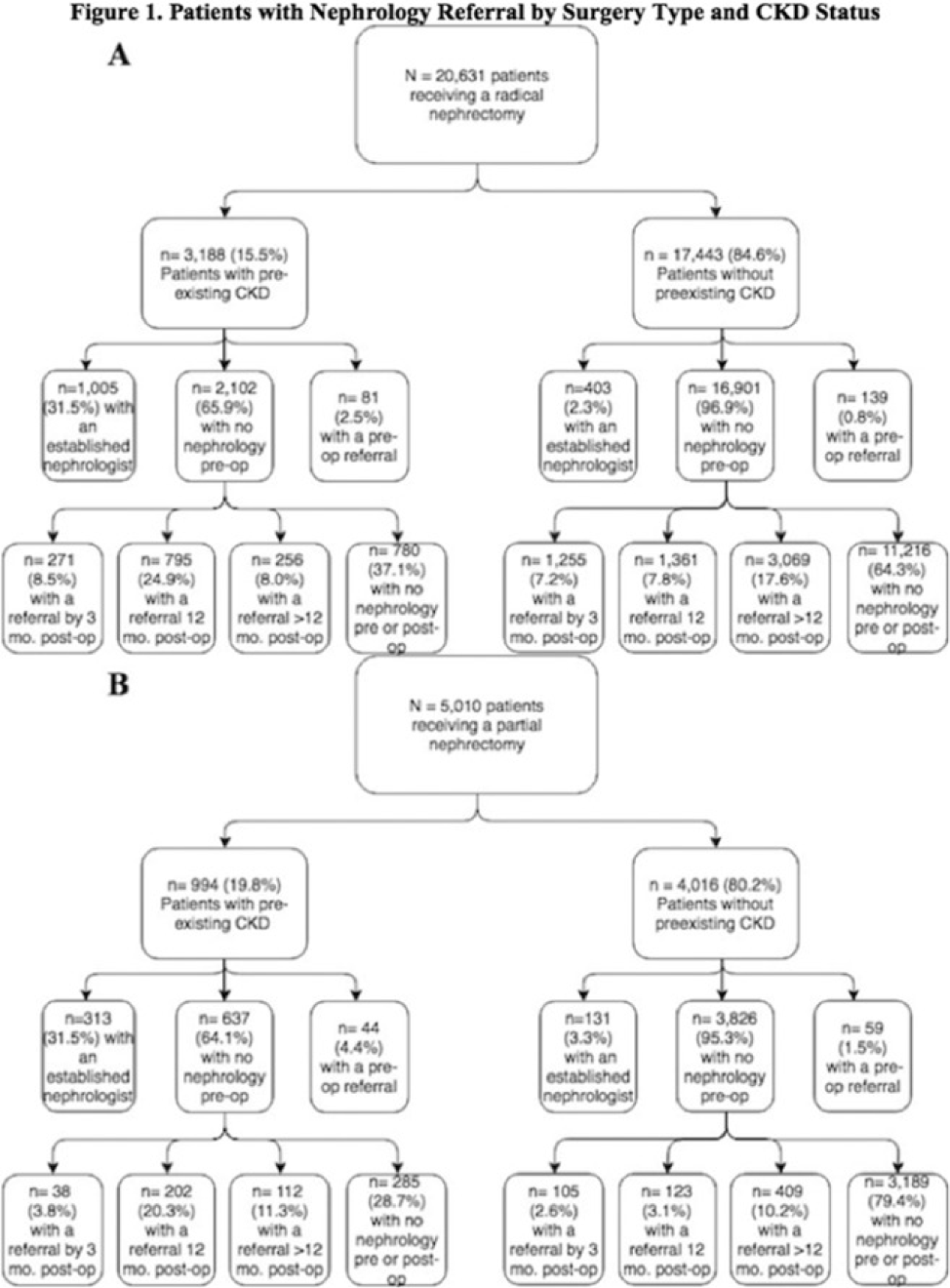
The authors identified a number of predictors associated with pre-operative referral including Stage III disease (OR: 1.27, CI: 1.10-1.48), higher Charlson Comorbidity Index scores (OR: 1.70, 95% CI: 1.40-2.05), and all stages of pre-operative CKD diagnosis, peaking with Stage 4 disease, (OR: 17.4, 95% CI: 8.72-34.74). With respect to post-operative referrals in the year following surgery, the following predictors were identified: diabetes (OR: 1.35, 95% CI: 1.17-1.56), radical nephrectomy (OR: 1.80, 95% CI: 1.43-2.26), and CKD stage at 12 months, with peak odds of nephrology referral associated with stage 4 CKD (OR: 21.84, 95% CI: 12.1-39.5).
There was no survival difference (HR= 0.97, 95% CI: 0.88-1.08) for patients with pre-operative referral or post-operative referral by twelve months (HR: 1.04, 95% CI: 0.96-1.13).
The authors conclude that few patients at risk for CKD development or progression receive nephrologic care prior to nephrectomy. However, pre-operative consultation did not appear to confer a survival benefit, though there may be residual confounding.
Presented by: Julia Wainger, MD, Johns Hopkins Medicine, Baltimore, MD, USA
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, Nashville, TN, USA, Twitter: @WallisCJD, at the 2020 American Urological Association (AUA) Annual Meeting, Virtual Experience #AUA20, June 27-28, 2020.


