By most guidelines, men undergoing radical prostatectomy by any approach classifies a patient as high-risk, with Caprini scores typically ≥5. However, no level-one evidence is available evaluating perioperative pharmacologic prophylaxis after radical prostatectomy for prostate cancer to prevent venous thromboembolism leading to significant practice variation across countries, centers, and individual surgeons. At the American Urological Association (AUA) 2020 virtual annual meeting, Hiten Patel, MD, MPH, and colleagues reported results of their trial assessing the impact of pharmacologic prophylaxis on the incidence of symptomatic venous thromboembolism and adverse events after radical prostatectomy with a secondary objective of evaluating overall venous thromboembolism in a screening subcohort.
This was a prospective, phase 4, single-center, randomized trial conducted between July 2017 and November 2018 at the Johns Hopkins Hospital and Johns Hopkins Bayview Medical Center. Adult men with prostate cancer undergoing open or robotic-assisted laparoscopic radical prostatectomy were randomized to pharmacologic prophylaxis (subcutaneous heparin (5,000 units) <2 hours before surgery and every 8 hours postoperatively until discharge) versus routine care alone (intermittent pneumatic compression devices, encouragement of early ambulation). The screening subcohort was offered a lower extremity duplex ultrasound at 30-days post-operatively. The primary efficacy outcome was the incidence of symptomatic venous thromboembolism (pulmonary embolism or deep venous thrombosis). Primary safety outcomes included the incidence of symptomatic lymphocele, symptomatic hematoma, or bleeding after surgery. Secondary outcomes were overall venous thromboembolism, estimated blood loss, total surgical drain output, complications, and surveillance imaging bias. As follows is the trial flow diagram: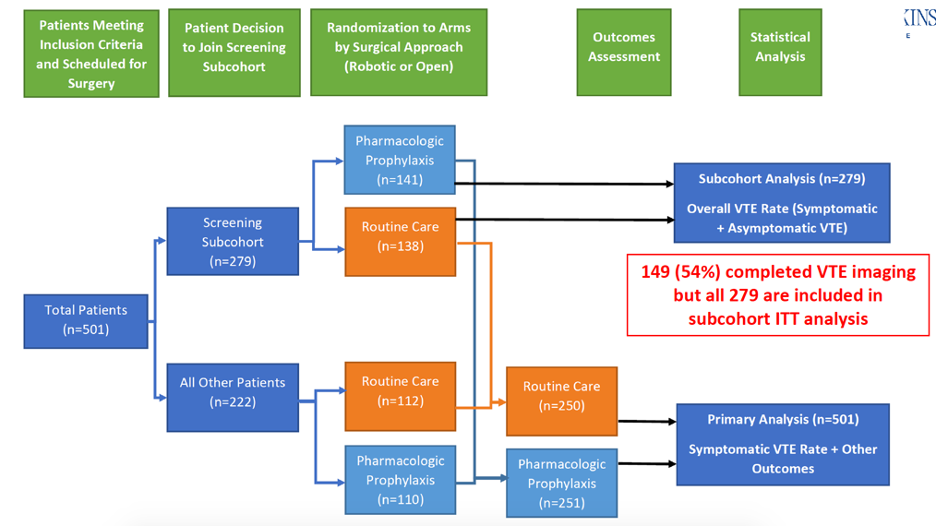
There were 501 patients (75.3% robotic) that were randomized and 99.8% (500/501) completed follow-up. Overall, 83.6% of patients underwent a pelvic lymph node dissection and 79.2% were ≥GG2 prostate cancer. At the second interim analysis (N=445), the symptomatic venous thromboembolism rate was 2.3% (4 pulmonary embolism plus deep vein thrombosis, 1 deep vein thrombosis) for routine care compared to 0.9% (1 pulmonary embolism plus deep vein thrombosis, 1 deep vein thrombosis) for pharmacologic prophylaxis (RR 0.40, 95% CI 0.08-2.03, p=0.268) meeting a futility threshold for early stopping. Among the screening subcohort, the overall venous thromboembolism rate was 3.3% vs. 2.4% (p=0.720). Results were similar at the final analysis (symptomatic venous thromboembolism: 2.0% vs. 0.8%, p=0.285; overall venous thromboembolism: 2.9% vs. 2.8%, p=1.00).
The following highlights the results of the subgroup analyses: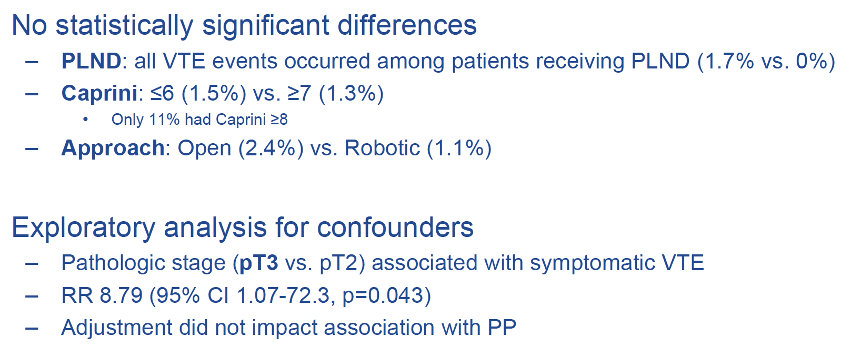
There were no differences in safety or secondary outcomes observed. Interestingly, all venous thromboembolism events (7 symptomatic, 3 asymptomatic) occurred in patients undergoing pelvic lymph node dissection.
The authors highlighted several limitations of the PREVENTER trial, PREvention of VENous ThromboEmbolism Following Radical Prostatectomy:
- This was a single-institution study with 75% of the cases being robotic
- It was underpowered for the event rate observed – based on the 2nd interim analysis, this would have required a sample size of >2,000
- Patients were not blinded
- There were few patients with Caprini scores ≥8
- The study did not require screening ultrasonography of all patients enrolled
Dr. Patel concluded his summary of the PREVENTER trial with the following concluding statements:
- Pharmacologic prophylaxis did not significantly reduce the rate of symptomatic or overall venous thromboembolism up to 30 days after radical prostatectomy
- However, there was no increase in the development of symptomatic lymphoceles, bleeding, or other adverse events
- Pharmacologic prophylaxis may be safely implemented when indicated for high-risk patients (Caprini scores ≥8) or patients receiving pelvic lymph node dissection
- These results may be applicable to other minimally-invasive surgeries with low morbidity and short hospital stays
Presented by: Hiten D. Patel, MD, MPH, James Buchanan Brady Urological Institute, Johns Hopkins Medical Institutions, Baltimore, MD, USA
Co-Authors: Farzana Faisal, Bruce Trock, Gregory Joice, Zeyad Schwen, Philip Pierorazio, Michael Johnson, Trinity Bivalacqua, Misop Han, Michael Gorin, H. Ballentine Carter, Alan Partin, Christian Pavlovich, Mohamad Allaf
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, twitter: @zklaassen_md, at the 2020 American Urological Association (AUA) Annual Meeting, Virtual Experience #AUA20, June 27- 28, 2020.


