As ICI therapy is relatively new, in this time frame they identified only 367 patients treated with ICI at any point during their systemic therapy treatment – of whom, 232 had CN and 135 had systematic therapy (ST) alone. The breakdown is seen below:

Of note, ICI therapy was first line in 28.1%, second line in 17.4%, and 3rd line or later in the majority of patients (54.5%). This naturally does not reflect current practice where ICI therapy is often first line.
CN occurred a median of 0.9 months (IQR 0.4 – 1.9) after mRCC diagnosis if it did occur.
When looking at the patient population, patients in both groups differed in a few key metrics:
- IMDC risk classification: In the CN group, IMDC was Favorable, Intermediate or Poor in 5.6%, 65.4%, and 16.4%, respectively, compared with 2.9%, 65.4%, and 29.4% in ST (p= .01).
- Number of metastases: Patients had one site of metastasis in CN: 55.6% vs. ST: 34.6% (p=.002).
- Age: Patients undergoing CN were younger at the time of metastatic disease, age 60 (CN) vs. 62 (ST)
- Histology: In the CN group, 9.1% non-clear cell histology vs. 18.5% non-clear cell histology in ST group.
Looking at responses:
- In patients undergoing CN and 1L ICI therapy, 19.2% had complete response, 27.6% partial response, 23.4% stable disease, and 19.2 had progressive disease vs. 0%, 26.8%, 17.9%, and 32.1% respectively in ST patients (p=.003)
- Median OS in the CN group was 56 months (95% confidence interval [CI], 50–77) vs. 19 months in ST group (95% CI 12 – 23, p<.0001).
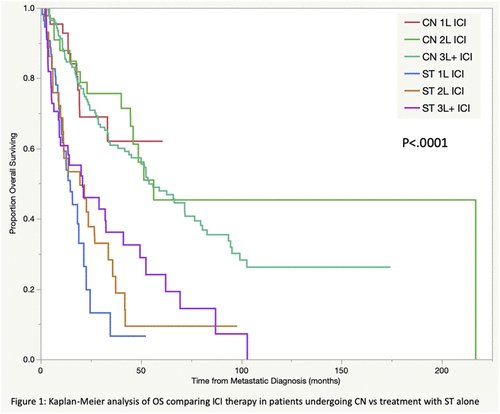
On multivariable analysis, CN was associated with improved OS (HR 0.32, p<.0001) – the benefit was even stronger in patients receiving ICI first line (HR 0.22, p < 0.001). Looking at the KM curves below, regardless of line of therapy from ICI standpoint, patients who underwent CN had better overall survival.
This is further broken down in the data presented during their talk:
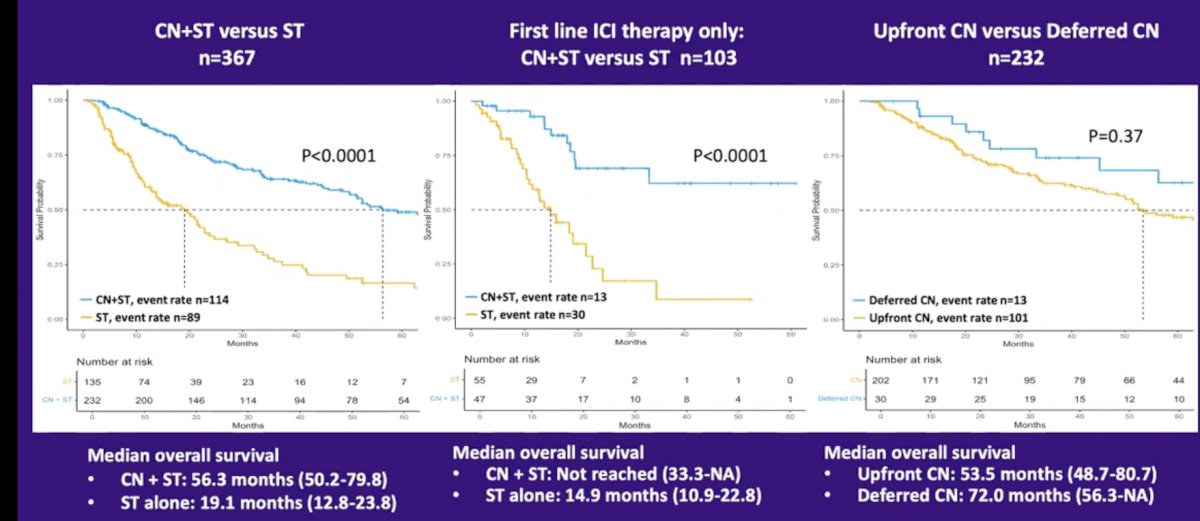
The timing of CN did not seem to affect outcomes. But, as discussed earlier, the CN benefit was seen in the entire cohort and in the patients that underwent ICI therapy in the first line.
However, this study is fraught with the same significant limitations that all retrospective series is limited by – patient selection. Patients who underwent CN were likely healthier (not directly measured in this study), had better IMDC risk stratification, had less metastatic burden, and therefore were always likely to do better. Also, this study is not limited to patients getting ICI in the first line – so this may not be a generalizable conclusion.
Important work, but likely not practice-changing. Ongoing randomized clinical trials look at the role of upfront ICI or perioperative ICI will be revealing.
Presented by: Evan Gross, BA, Medical Student (3rd year) at the University of Washington
Written by: Thenappan (Thenu) Chandrasekar, MD – Urologic Oncologist, Assistant Professor of Urology, Sidney Kimmel Cancer Center, Thomas Jefferson University, @tchandra_uromd on Twitter during the 2021 American Urological Association, (AUA) Annual Meeting, Fri, Sep 10, 2021 – Mon, Sep 13, 2021.


