(UroToday.com) In the Society of Urologic Oncology (SUO) plenary session held at the American Urologic Association (AUA) Virtual Annual Meeting, Dr. Zachary Klaassen addressed the question of suicidality in urologic cancer patients. After many years of little attention, there has been increasing interest in understanding the mental health of patients with cancer.
Dr. Klaassen began by highlighting that mental health illness is common among patients with urologic cancers. Considering first prostate cancer, more than one-fifth of patients with localized disease develop mental health illness in the 4 years following diagnosis. Further, both treatment with surgery and radiotherapy were associated with increased use of anti-depressants while longer durations of androgen deprivation therapy were associated with an increasing rate of depression. Among those with bladder cancer, more than half of patients with non-metastatic disease were prescribed a psychotropic medication following diagnosis and a similar number sought care for a psychiatric disorder.
Mental health disorders may culminate in suicidality. Highlighting his own analysis from 2015, Dr. Klaassen cited data from the SEER registry which identified 2268 patients who died of suicide among just over 1.2 million patients with urologic cancers. This risk was highest among patients with bladder cancer undergoing cystectomy but other risk factors included Caucasian race, male gender, elderly, and those with more advanced disease. An updated analysis from SEER found a similar proportion of patients dying of suicide.
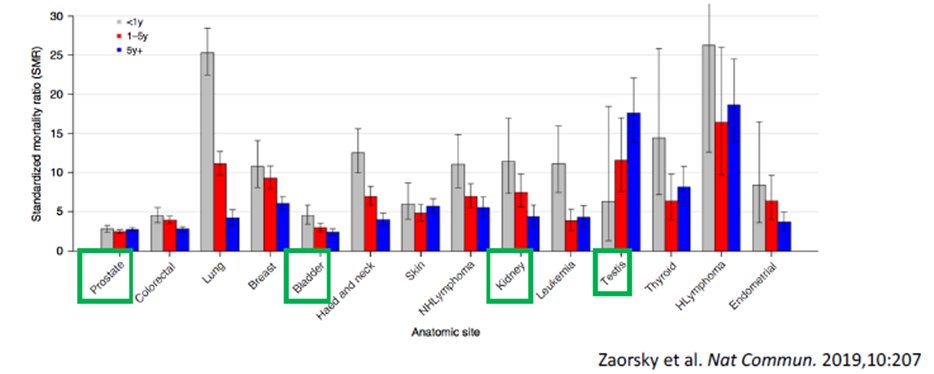
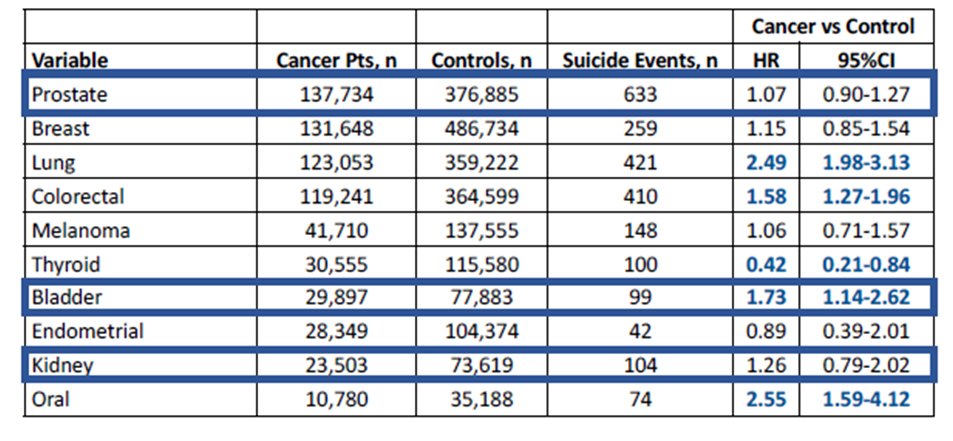
Dr. Klaassen then emphasized that in total there are 25 population-level studies examining suicide rates among cancer patients. However, none of this addressed baseline (ie. pre-cancer diagnosis) mental health. He, therefore, highlighted his own work which accounted for this. Among patients with the 10 most common incident solid organ malignancies in Ontario, Canada (and matched to non-cancer controls), he showed that there was an increased risk of suicide in the first 5 years or so following cancer diagnosis, an effect which subsequently attenuated. Interestingly, the effect of cancer diagnosis was most prominent among those with little mental health illness at baseline whereas this was not significant among those with more severe mental health illness prior to cancer diagnosis. Among the urologic malignancies, he showed data suggesting that the effect of cancer diagnosis on suicidal death was significant only among those with bladder cancer. Outside of urology, patients with lung, colorectal, and oral cancers appeared also to be at increased risk of suicide.
Transitioning from the data emphasizing the importance of mental health and suicide among cancer patients, Dr. Klaassen emphasized the need and urgency for cancer survivorship programs to address the mental health needs of our patients. In particular, he began by citing data from a survey aimed at identifying patients at risk of suicide. A number of important barriers were identified including that many patients give no warning or conceal their suicidality, those most at risk may not return for follow-up, a lack of time, a physician/professional fear of asking, a lack of training or awareness, and a lack of resources to offer these patients. However, the article also suggested a number of important strategies that may be employed including paying attention to both verbal and nonverbal indicators, identifying those at elevated risk based on a history of mental health disorders or other characteristics, being attuned to mental health distress, and the importance of acknowledgment and explicit actions. He then emphasized the NCCN distress thermometer which is included in their guidelines for the management of patients with cancer.
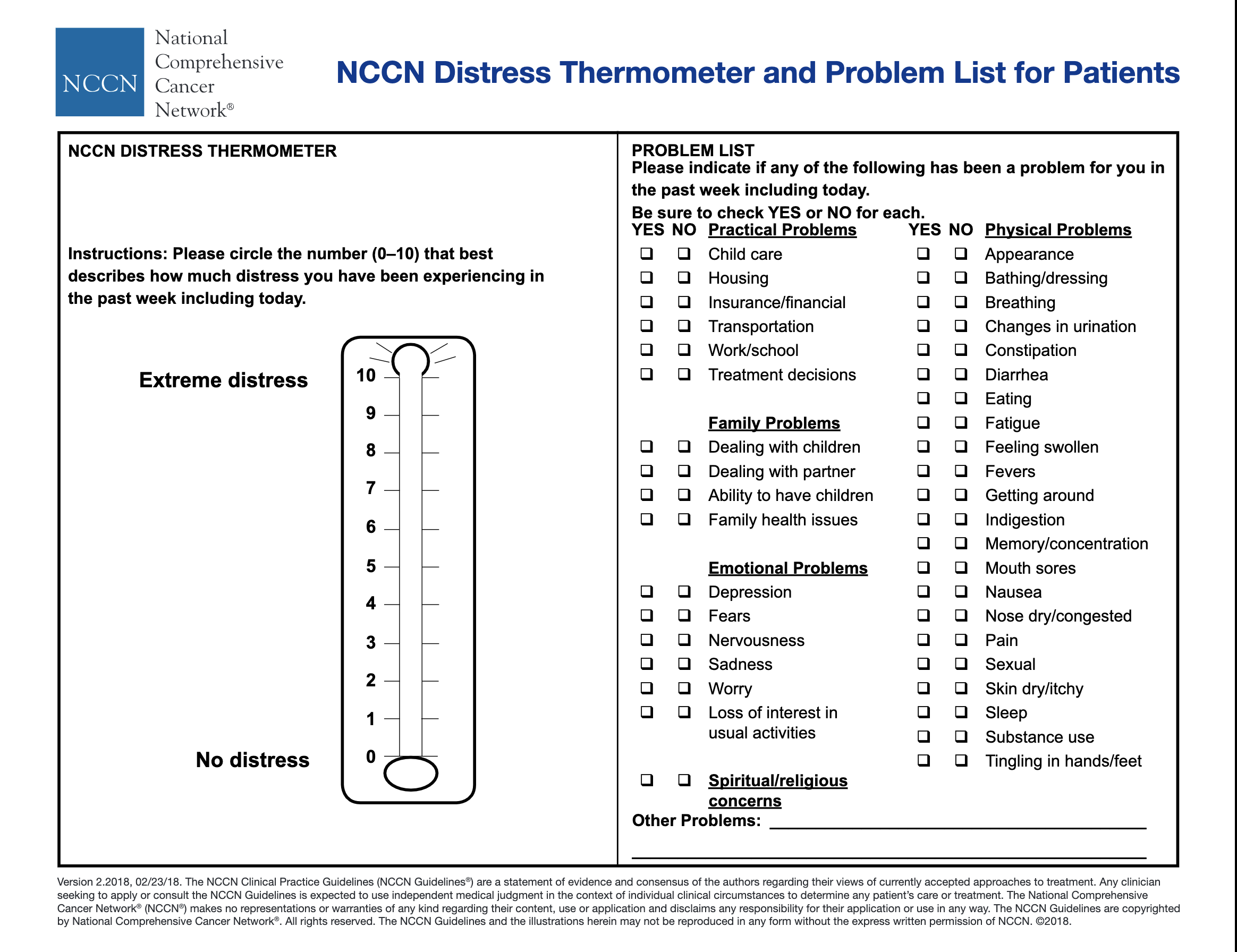
Looking forward, Dr. Klaassen suggested that we may improve outcomes in the continuum of our care of the patient with cancer. Beginning at a new patient intake, we should be attuned to a psychiatric history, not just cancer-related details. Further, being aware of recent psychiatric utilization may point to an increased risk. In ongoing follow-up, we need to embrace routine screening for distress, depression, and suicidal ideation. Further, when needed, we must initiate appropriate referrals for psychological or psychiatric evaluation.
Presented by: Zachary Klaassen, MD, Urologic Oncologist, Assistant Professor Urology, Residency Program Director, Ronald W. Lewis, MD Endowed Chair for Urologic Education, Director of Urologic Oncology and Clinical Urological Research, Medical College of Georgia at Augusta University; Georgia Cancer Center
Written by: Christopher J.D. Wallis, University of Toronto, Twitter: @WallisCJD during the 2021 American Urological Association, (AUA) Annual Meeting, Fri, Sep 10, 2021 – Mon, Sep 13, 2021.


