(UroToday.com) In a plenary session entitled “Advances in Prostate Cancer: Androgen Deprivation Therapy Across the Disease Continuum” held in conjunction with the American Urologic Association Virtual Annual Meeting this evening, Dr. David Penson explored advances in non-metastatic castration resistant prostate cancer (nmCRPC).
Dr. Penson began by emphasizing that PSA doubling time is strongly associated with the risk of metastasis and death in patients with nmCRPC. In particular, there is an infection of the curve around 7 months. However, most have categorized the risk based on a threshold of 10 months.
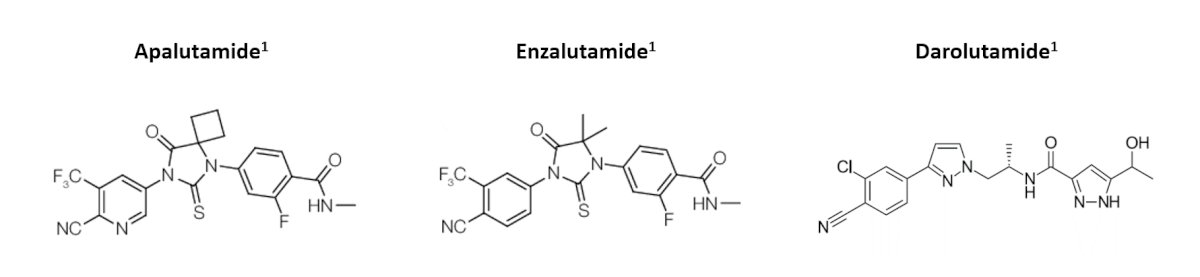
Notably, in this disease space, work from the ICECaP cohort demonstrated the metastasis-free survival is a valid surrogate for overall survival. Thus, this became a regulatory approved endpoint and formed the basis for approval of novel treatment approaches in this disease space. Three next-generation androgen receptor inhibitors have been subsequently approved for this indication. Apalutamide and enzalutamide are structurally similar which darolutamide is distinct and, as a result, has lower blood-brain barrier penetration.
Dr. Penson then compared and contrasted the three trials which assessed these agents. Despite overall similarities in design and conduct, there are some differences, particularly as they relate to inclusion criteria, the use of bone targeting agents, the selection of secondary endpoints, and cross-over unblinding.
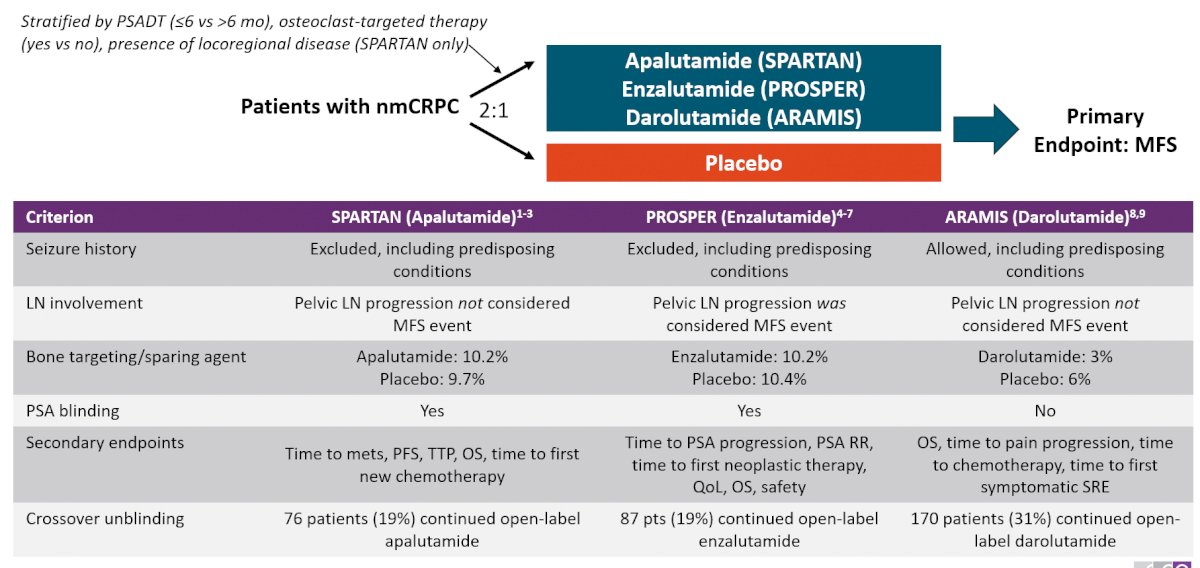
Despite these differences, the results of the three studies are remarkably similar. Each study demonstrated a significant improvement in the primary outcomes of metastasis-free survival with approximately 22-24 months overall median improvement in metastasis-free survival. Further, assessing the overall survival data, each trial demonstrated significantly improved results for the early addition of a next-generation androgen receptor inhibitor, though cross-trial comparisons don’t allow for a direct head-to-head comparison of the agents.
In terms of toxicity, Dr. Penson emphasized that fatigue, falls, and fractures are among the most important events for patients receiving these agents. In terms of managing these when considering the use of enzalutamide, he suggested that it shouldn’t be used in those patients with a seizure history and that care should be taken if patients are prescribed strong CYP2C8 inhibitors or other CYP-inducing agents. In terms of apalutamide, rash and hypothyroidism are somewhat unique toxicities though may be managed relatively easily. In terms of darolutamide, fatigue may necessitate dose reduction, and rash, while rare, can be managed in much the same way as with apalutamide.
Based on these data, NCCN guidelines for nmCRPC recommend continued ADT for all men. For those with PSA doubling times more than 10 months, observation is recommended. However, for those with a shorter PSA doubling time, treatment with one of these next-generation androgen receptor inhibitors is recommended.
Dr. Penson then moved on to discussing the cardiovascular events of these oral agents. In particular, though rates are relatively low in these trials, major cardiovascular events were noted in SPARTAN and PROSPER, including both patients in the intervention and control arms. A meta-analysis assessing the safety of these agents found an increased relative risk of both cardiovascular events (RR 2.44) and adverse event-related deaths (RR 4.87). However, this risk is not necessarily consistent for all patients. In particular, he highlighted data based on the SEER-Medicare dataset demonstrating that men with more cardiovascular risk factors at the time of initiating treatment had increased risks of mortality. Thus, he suggested that all patients should be screened for cardiovascular disease and diabetes. Optimal care of these patients will likely require multidisciplinary teams with careful attention to adverse events.
He then transitioned the discussing bone health, first noting the AUA guidance on this topic. The AUA guidelines recommend discussing the risk of osteoporosis associated with ADT and initiating preventative measures including supplemental calcium and vitamin D, smoking cessation, and exercise. Additionally, pharmacotherapy may be added for patients with high fracture risk. Highlighting the seminal data from Shahinian in 2005, he emphasized that the duration of ADT is strongly associated with the risk of fracture and fracture requiring hospitalization. Meta-analysis has demonstrated that supplemental vitamin D may reduce the hip fracture risk of 26% and non-vertebral fracture risk by 23%, though these effects are significant only when doses of 700-800 IU/day are used. The use of supplemental calcium is less evidence-based though is critical for men who are on zoledronic acid or denosumab. These agents may improve bone mineral density in men with nmCRPC.
Dr. Penson then moved to the question of nmCRPC as a shrinking disease state. This is driven by the fact that it is defined based on imaging. As a result, early use of next-generation imaging is likely to detect radiographic evidence of metastatic disease in many patients who are nmCRPC according to conventional imaging.
Presented by: David Penson, MD, MPH, MMHC, Vanderbilt University Medical Center
Written by: Christopher J.D. Wallis, University of Toronto Twitter: @WallisCJD during the 2021 American Urological Association, (AUA) Annual Meeting, Fri, Sep 10, 2021 – Mon, Sep 13, 2021.


