(UroToday.com) The 2023 American Urological Association (AUA) annual meeting held in Chicago, IL between April 28 and May 1st, 2023, was host to a non-invasive bladder cancer moderated poster session. Dr. Karsten Zieger presented the results of an analysis from the Nordic registry evaluating the role of flexible blue light cystoscopy in the surveillance of non-muscle invasive bladder cancer.
Non-muscle invasive bladder cancer (NMIBC) accounts for approximately 75% of newly diagnosed bladder cancer cases. Patients with NMIBC undergo frequent, occasional lifetime, surveillance cystoscopies due to the recurrent nature of this field disease. Blue light enhancement, when compared to standard white light cystoscopy, has been demonstrated in numerous studies to improve the sensitivity, and, to a lesser degree, the specificity of cystoscopic evaluations.1 This study aimed to further evaluate the performance of blue light flexible cystoscopy (BLFC) in the surveillance setting.
The authors utilized The Nordic Blue Light Flexible Cystoscopy (BLFC) registry, which is a prospective, observational, multi-center study including patients undergoing BLFC for suspicion or surveillance of NMIBC in an outpatient setting. Available, recorded data included patients’ demographics, patients’ bladder cancer history, findings on blue light and white light cystoscopies, patients’ preferences, discomfort, and treatments.
This study included a total of 319 patients undergoing surveillance for NMIBC, with a total of 436 BLFCs performed. Patients were risk stratified per the EAU classification as follows:
- High risk: 54%
- Intermediate risk: 43%
- Low risk: 3%
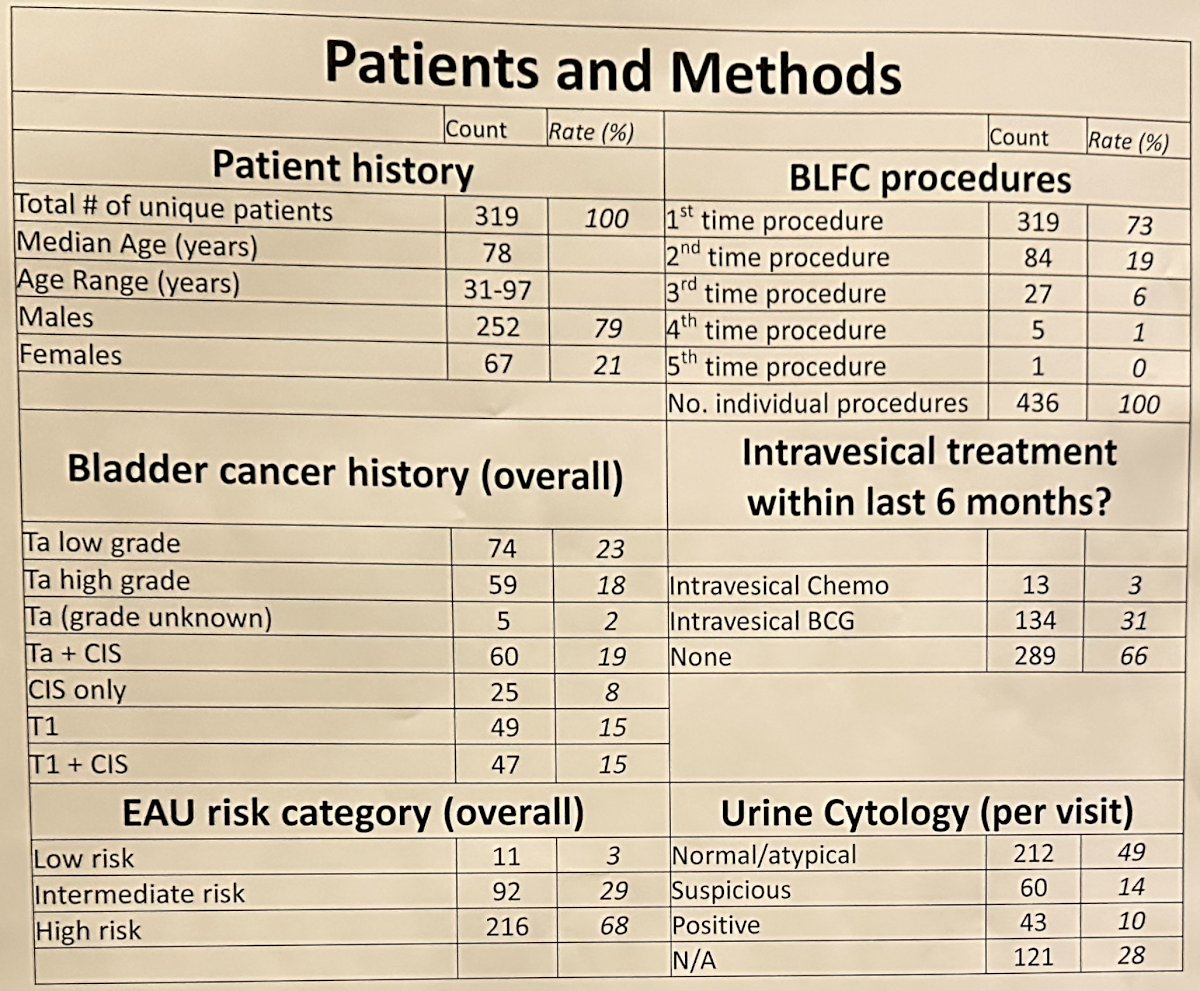
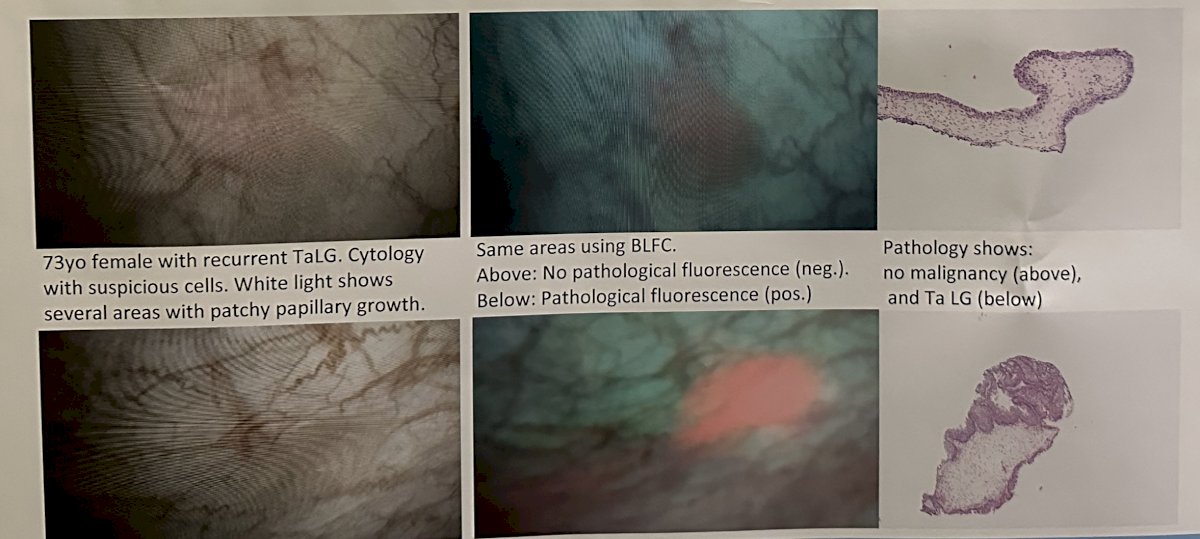
With respect to previous intravesical adjuvant therapy, 34% of patients had received BCG or intravesical therapy prior to BLFC. 318 (73%) cystoscopies, using blue or white light, demonstrated suspicious lesions. 452 lesions were biopsied, of which 409 and 43 were blue light positive and negative, respectively. Of these lesions, 31% and 16% were positive for malignancy, respectively.
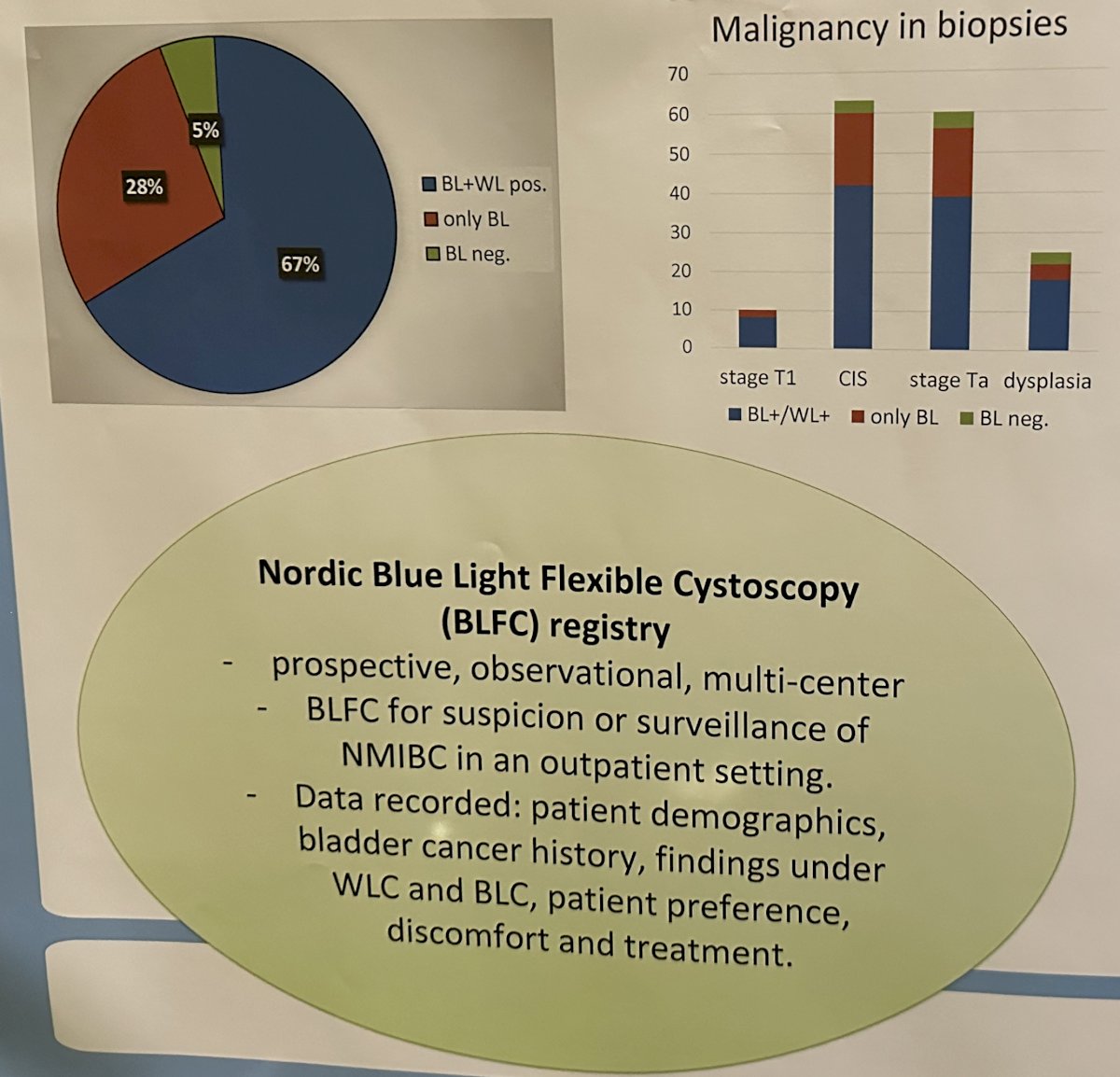
In 86 cases (20%), lesions were identified only by blue light examinations. Pathology showed malignancy in 37/104 biopsies performed (36%), including 18 cases of CIS. Patients with small recurrences underwent office fulguration, whereas 45 patients (10%) were referred to TURBT, and 82 patients subsequently received adjuvant intravesical therapy.
34 patients expressed discomfort during BLFC, due to bladder distension or the associated biopsy and/or fulguration. Physicians reported the benefit of BLC in 367/436 (84%) of the cystoscopies, with the main advantage being stronger confidence in confirming or refuting a suspicious lesion.
Dr. Zieger concluded that flexible blue light cystoscopy, as an adjunct to white light cystoscopy for surveillance of NMIBC, improves the detection of malignant lesions. Furthermore, it may improve the surgeons’ confidence in identifying clinically important lesions. Dr. Zieger suggested that the combination of BLC with immediate fulguration of tumors in an outpatient setting may positively affect the NMIBC patients’ treatment/surveillance burden.
Presented by: Karsten Zieger, MD, PhD, Consultant Urologist, Urological Research Center, Vejle Hospital, Lillebaelt Hospital, University Hospital of Southern Denmark, Vejle, Denmark
Written by: Rashid K. Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 American Urological Association (AUA) annual meeting held in Chicago, IL between April 28 and May 1st, 2023
Reference:
- Daneshmad S, et al. Blue light cystoscopy for the diagnosis of bladder cancer: Results from the US prospective multicenter registry. Urol Oncol, 2018.


