(UroToday.com) The 2023 American Urological Association (AUA) annual meeting held in Chicago, IL between April 28 and May 1st, 2023, was host to a non-invasive bladder cancer podium session. Professor Rakesh Heer presented results from the PHOTO trial evaluating whether previous experience with blue light cystoscopy can improve a surgeon’s white light resection performance.
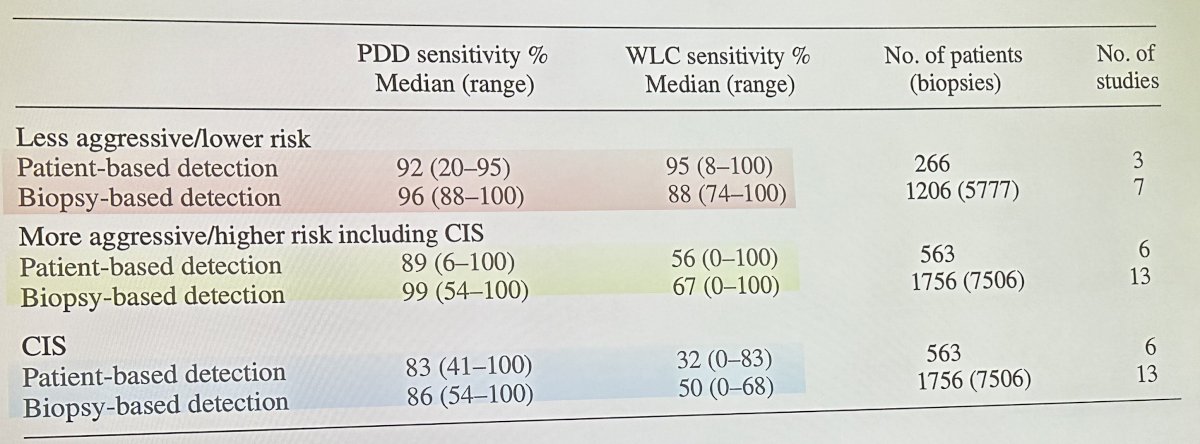
Professor Heer began by noting that incomplete resection of bladder tumors likely contributes to 20-40% of observed recurrences. As such, improved visualization of all tumor present with photodynamic diagnosis (PDD) may allow for improved maximal resection and, thus, lower recurrence rates. The benefit of PDD is most pronounced in patients with more aggressive/higher risk disease as demonstrated in the table below:
Following the results of early reports evaluating PDD in this setting, the NIHR (National Institute for Health and Care Research) recommended performing a new study focusing on higher risk patients that would evaluate the efficacy and cost-effectiveness of PDD in a real-world setting using contemporary management options, including intravesical chemotherapy and BCG, with long-term outcomes assessments planned.
PHOTO is a pragmatic RCT with a primary outcome of time to recurrence at 3 years. This study included 22 sites with 538 participants enrolled between 2014 and 2018. The median follow-up in this study was 44 months.1 
This study failed to meet its primary endpoint of time to recurrence at 3 years follow-up, with 3-year recurrence-free rates of 58% and 62% in the PDD and white light groups, respectively (HR: 0.94, 95% CI: 0.69 – 1.28, p=0.70). Furthermore, no significant benefits were seen for rates of progression to muscle-invasive disease, overall survival, or bladder cancer-specific mortality. 
Even after an extended follow-up of 18 months, no differences were observed in recurrence rates between the two arms.
However, when stratified by surgeon experience, as categorized below, we see that the recurrence rates for both modalities decreased as surgeon experience improved.
This is further demonstrated in the Kaplan Meier curve below with outcomes stratified by surgeon experience demonstrating lower recurrence rates with increased surgeon experience.
Professor Heer concluded that real-world PDD versus white light-guided TURBT for primary intermediate or high risk NMIBC demonstrates no difference in recurrence over 3 years. He hypothesized that this may be secondary to the learning curve for PDD and a bystander effect on white light cystoscopy. He emphasized that the role of PDD is rapidly growing and is currently refining the standard TURBT training methods.
Presented by: Professor Rakesh Heer, MD, PhD, Professor, Chair of Urology, Department of Surgery and Cancer, Imperial College London, London, UK
Written by: Rashid K. Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023
Reference:
1. Heer R, et al. A Randomized Trial of PHOTOdynamic Surgery in Non–Muscle-Invasive Bladder Cancer. NEJM Evidence, 2022.


