(UroToday.com) The 2023 American Urological Association (AUA) annual meeting held in Chicago, IL between April 28 and May 1st, 2023, was host to an invasive bladder cancer podium session. Dr. Domenique Escobar presented the results of the analysis evaluating the use of 68Ga-FAP-2286 PET imaging in patients with localized bladder cancer.
Given the limitations of currently available imaging modalities (i.e., CT, MRI, FDG-PET) for bladder cancer staging, there is an urgent need for advances in imaging technology to ensure accurate staging and treatment.
Cancer-associated fibroblasts (CAFs) express cell surface proteins such as fibroblast activation protein-α, a peptidase that plays a major role in the tumor microenvironment by remodeling the extracellular matrix. CAFs in the stromal microenvironment support growth and invasion of epithelial cells by the secretion of cytokines, chemokines, and extracellular matrix components that promote cell transitions and metastasis. A 2014 meta-analysis demonstrated that FAP overexpression in fibroblasts surrounding several malignancies was associated with lymph node metastases and poorer prognosis. As such, FAP may be an important target in the evaluation and treatment of patients with various cancers.

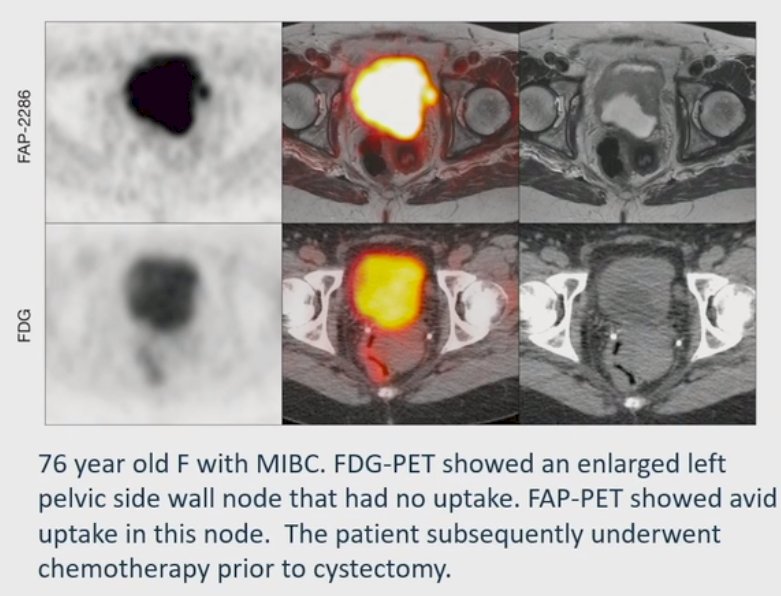
This has been previously evaluated in the bladder cancer disease space, across clinical stages, with 8 patients undergoing both an FDG-PET and a FAP-PET. There was note of significantly higher uptake in the FAP-PET images compared to FDG-PET, with higher mean SUVmax and FAP-PET detecting 9 lesions that were missed by FDG-PET.1 A further study of 15 patients who underwent both a FAP-PET and CT scan found that in 4/15 patients, there were lesions on FAP-PET that were missed on standard CT imaging. In addition, 2/15 patients had pulmonary nodules and pelvic lymph nodes suspicious for metastatic spread on CT, but without increased uptake on FAP-PET, which were subsequently found to be negative for malignancy.2
The objective of this pilot study was to assess the diagnostic performance of 68Ga-FAP-2286 (FAP)-PET imaging in a small cohort of patients with bladder cancer at a single institution (UCSF).
This report included patients with solid tumors who underwent a FAP-PET within the context of a clinical trial (NCT04621435), including 16 patients with bladder cancer, of whom 10 had clinically localized disease treated with curative intent at the time of imaging. All patients underwent standard imaging with CT, MRI, FDG-PET, or bone scan within 8 weeks of FAP-PET. The SUVmax and size of FAP-PET-positive lesions, defined as any focus of activity with ≥1.5 times higher SUV compared with mediastinal blood pool, were documented.
The results are demonstrated below. In brief, the age range was 28 to 90, 9/10 were men, and 8/10 had cT2-3 disease.
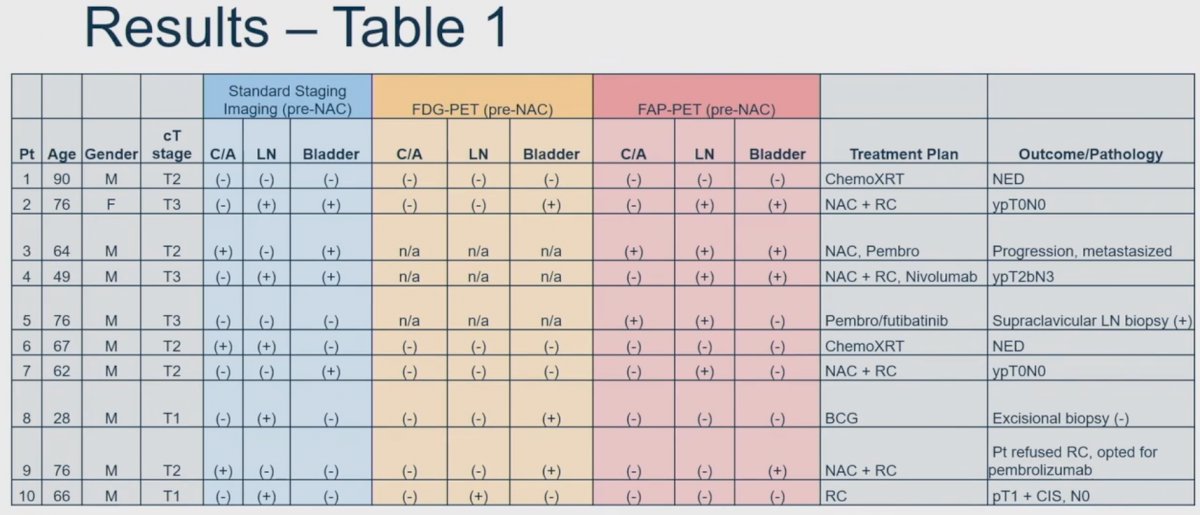
The concordance of the 12 FAP-PET scan was 33% with standard imaging (CT/MRI) and 43% with FDG-PET. Of the 8 patients with pathologic or radiographic follow-up available, FAP-PET was concordant with true disease status in all 8 patients. Significantly, it appears that FAP-PET may be of utility in predicting the presence of pathologic nodal disease in patients undergoing NAC and may alter management in select cases:
- One had resolution of LN uptake pathology at cystectomy was ypT0N0
- One had decreased but persistent uptake pathology at cystectomy was ypT2bN3.
Based on these results, Dr. Escobar concluded that:
- FAP may be an important diagnostic target in bladder cancer with improved accuracy compared to conventional imaging and FDG-PET
- FAP likely has a higher specificity that conventional imaging techniques – in this cohort, inflammatory (false positive) nodes did not show uptake
- FAP-PET has the potential to change treatment pathways and improve patient care by better identifying metastatic sites or false positive lymph nodes in cancers considered clinically localized and by improving the assessment of response to systemic therapy
- Future studies evaluating the impact of improved imaging accuracy on patient outcomes are needed
- FAP may also be a target for radioligand therapy and ongoing studies are evaluating this
Presented by: Domenique Escobar, MD, Resident Physician, Department of Urology, University of California in San Francisco, San Francisco, CA
Written by: Rashid K. Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023
References:- Novruzov E, et al. Head-to-head Intra-individual Comparison of [68Ga]-FAPI and [18F]-FDG PET/CT in Patients with Bladder Cancer. Mol Imaging Biol, 2022.
- Unterrainer LM, et al. Feasibility of [68Ga]Ga-FAPI-46 PET/CT for detection of nodal and hematogenous spread in high-grade urothelial carcinoma. Eur J Nucl Med Mol Imaging, 2022.


