(UroToday.com) The 2023 AUA annual meeting included the Bladder Cancer Forum, featuring a debate discussing optimizing BCG therapy and managing BCG toxicity. Dr. Joshua Meeks started with a case of a 74 year old male with T1 high grade urothelial carcinoma + CIS on TURBT, with a subsequent negative re-TURBT four weeks later. He had some urgency and frequency that worsened after his first and second TURBT, however he did undergo six doses of induction BCG associated with severe irritation. His first cystoscopy after treatment showed erythema and reaction around the whole bladder, and he is currently up every 30 min at night to urinate, describing his current quality of life as “miserable”. He does want to receive additional BCG because of fear of cancer return, so he was treated with three more doses and now describes lower pelvic pain and burning with urination. Additionally, his creatinine is now up to 2.36 from 1.3 at baseline. A CT scan showed bilateral hydronephrosis down to the level of the bladder. Biopsies of the bladder demonstrated inflammation and granuloma.
Dr. Meeks than polled the audience asking “What would you recommend?”
- 57%: Stop all BCG
- 20%: Treat with an anti-TB medication
- 7%: ID referral
- 17%: Cystectomy
Dr. Badrinath Konety then discussed managing BCG toxicity. Historical studies suggest that BCG is quite a bit more toxic than intravesical chemotherapy such as epirubicin: 41% hematuria vs 28%, 36% urinary frequency vs 15%, and 24% severe dysuria vs 10%. Additionally, the rate of systemic toxicity necessitating stopping therapy for BCG may be as high as 28%, compared to only 4% for epirubicin. Additionally, there are several other rare, serious toxicities including (i) abscesses, (ii) arthritis, (iii) infected aneurysms, (iv) retrobulbar granuloma, (v) miliary lung infection, (vi) hepatitis and AV fistula (vii) delayed bladder ulcers, and (viii) mycotic aneurysms.
For persistent irritative symptoms (>48 hours +/- fever or malaise), Dr. Konety recommends considering the use of a fluoroquinolone and holding further BCG and treatment until symptoms have resolved. Several trials have assessed agents to try reducing BCG related irritative symptoms. In EORTC 30911, there was no benefit from INH, but there was an increase in LFTs when using INH for this indication. Oxybutinin has been tried with no effect to date. Ofloxacin (q6 hours and 18 hours post viding following BCG) and prurifloxacin (given q6 hours, 30 hours, and 54 hours post voiding BCG) have been assessed with reasonable results. Dr. Konety also notes that it may be reasonable to try nitrofurantoin 200 mg + tetracaine HCL 1 g + 6 methylprednisolone 165 mg mixed in 1L of distilled water. He notes that this is similar to a cocktail for interstitial cystitis, leading to a 94% reduction in nocturia and pain.
Systemic toxicity (temperature > 103F) occurs in ~3% of patients and leads to hospitalization. Patient should be treated with 300 mg INH + 600 mg rifampin daily +/- a fluoroquinolone. BCG sepsis should have 40 mg/day of prednisone added if symptoms fail to response, which helps with treating the hypersensitivity reaction. Patients should continue the 3 drug regimen for 3-6 months and further BCG is contraindicated.
Dr. Konety highlighted that there are several ways to prevent sepsis, including:
- Waiting at least 1-2 weeks from biopsy/TURBT to start BCG
- Do not give when patients are having gross hematuria
- Do not give if a patient is having a UTI (sterile bacteria is ok)
- Place the catheter atraumatically
- Drug preparation should be done meticulously in a sterile fashion
- Clinicians should have a prompt response to any changes in a patient’s condition
With regards to dose reduction, sometimes less is better, and even as little as 1/100 of a standard dose can generate a good response in the patient’s bladder. Dr. Konety advocates dose reduction in the face of toxicity rather than abandoning BCG (1/2, 1/3, 1/10, 1/30, 1/100, etc). Additionally, the dwell time can be reduced to 1 hour. Dr. Konety summarized the management of BCG toxicity with the following take-home messages:
- Local is the most common toxicity
- Sepsis is rare
- For local toxicity, it is reasonable to try a fluoroquinolone if symptomatic. Persistent fever and BCGosis should be treated with INH + rifampin and sepsis should have a three drug therapy + steroids
- Attention should be paid to timing and technique of instillation
- Dose reduction can reduce symptoms
Next, Dr. Wassim Kassouf discussed optimizing BCG therapy. He started his presentation by emphasizing that select NMIBC patients are very high risk, secondary to understaging and under estimating risk of progression, which leads to under treatment with BCG and potentially death from bladder cancer. According to the Canadian advanced urothelial carcinoma guidelines, upfront radical cystectomy should be offered to patients with high grade T1 disease with additional adverse tumor pathology features (level of evidence 3; strong recommendation):
- Variant histology (ie micropapillary, plasmacytoid, sarcomatoid)
- Presence of lymphovascular invasion
- Extensive invasion of the lamina propria or invasion into or beyond the muscularis mucosa (T1b/c)
- Presence of concomitant CIS in the bladder or prostatic urethra
- Multiple large (>= 3cm) tumors or persistent T1 high grade disease upon restaging TURBT
Patients receiving induction BCG should be optimized with maintenance BCG therapy. The classic Lamm 2000 SWOG study1 (6+3 protocol) consisted of 6-week BCG induction followed by a maintenance course consisting of 3 weekly treatments of BCG at 3, 6, 12, 18, 24, 30, and 36 months. BCG maintenance therapy increased recurrence free survival and worsening free survival.

Dr. Kassouf also highlighted that we should be optimizing dose and duration of BCG. In 2013, Oddens et al.2 published results of 1,355 patients with intermediate risk and high risk NMIBC randomized to 4 groups, with a median follow-up of 7 years. The 5-year disease free rates were:
- 54.5% on 1/3 dose for 1 year
- 58.8% on full dose for 1 year
- 62.6% on 1/3 dose for 3 years
- 64.2% on full dose for 3 years
A pre-specified decrease of 10% was only observed for the 1/3 dose for 1 year versus full dose for 3 years, with no differences in progression rates. A 3 year full dose was superior to 1 year 1/3 dose (HR 0.75, p = 0.01) in all comers. In the subgroups intermediate risk full dose for 1 year was similar to full dose for 3 years, and for high risk 3 years decreased recurrence versus full dose for 1 year.
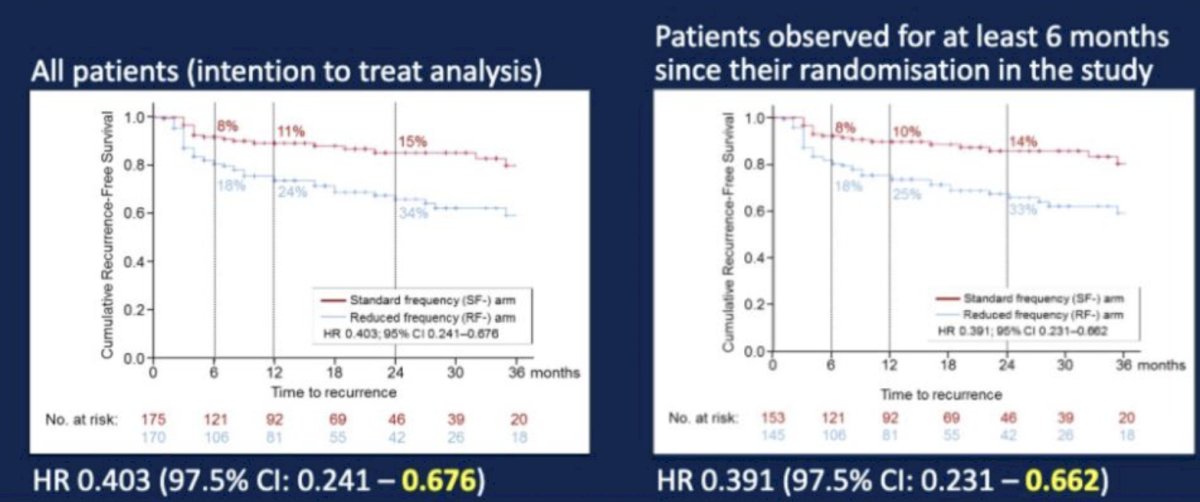
With regards to the optimal frequency of BCG, Dr. Kassouf highlighted the NIMBUS clinical trial presented by Marc-Oliver Grimm at GU ASCO 2020 whereby patients were randomized to induction BCG weekly (weeks 1-6) versus weekly (weeks 1, 2, and 6) followed by maintenance therapy for all patients (BCG weekly weeks 1-3; months 3, 6, and 12). The primary endpoint was time to first recurrence:

Time to first recurrence favored the standard frequency arm with a hazard ratio of 0.403 (97.5% CI 0.241-0.676) in the intention to treat analysis, and among patients observed for at least 6 months since their randomization (HR 0.391, 97.5% CI 0.231-0.662):
For assessing the impact of BCG strain, Rentsch et al.3 assessed 142 patients with high risk NMIBC who were randomized to 6 week induction of ImmuCyst (Connaught) vs OncoTice. Over a median follow-up of 25 months, ImmuCyst had superior: 5-year recurrence free survival (75% vs 48%; p = 0.01), 5-year progression free survival (94% vs 88%, p = 0.33), but with no survival difference. The SWOG 1602 treatment schema assessing different BCG strains is as follows:

Dr. Kassouf notes that 2023 marks the 50th anniversary of the first patient receiving BCG, and as such we are now building on BCG with novel combination therapy. In the QUILT 3.032 trial, all treated patients received intravesical N-803 plus BCG, consistent with the standard induction/maintenance treatment schedule. The primary endpoint for Cohort A (CIS) is incidence of complete response of CIS at any time. The primary endpoint for Cohort B (Papillary) is disease-free rate at 12 months. The trial design for QUILT 3.032 is as follows:
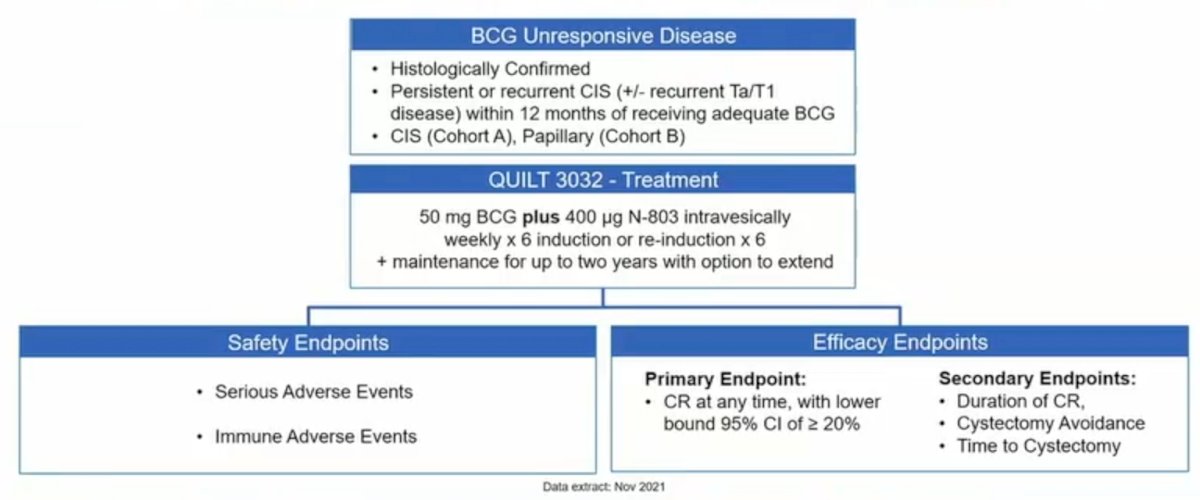
Among CIS patients, the complete response rate was 71%, with a complete response rate at 12 months of 45%. Furthermore, among patients with papillary disease in QUILT 3.032, the median DFS was 23.6 months, the DFS rate at 12 months was 57%, and the DFS rate at 24 months was 48%. This meets the given standard for these trials of 30% DFS rate at 12 months. In high-risk NMIBC that is BCG naïve, there are two BCG + immunotherapy trials, POTOMAC trial (Astra Zeneca; ongoing) and the B8011006 trial (Pfizer; pending).
Dr. Kassouf concluded his presentation for optimizing BCG therapy with the following take-home messages:
- Risk stratification is important for high-risk NMIBC
- We should be trying for maintenance therapy for the majority of our patients
- Duration, dose and frequency are important
- At this point in time the question regarding BCG strain remains unanswered
- Novel combination therapy remains an exciting possibility
Moderator: Joshua J. Meeks, MD, PhD, Northwestern University School of Medicine, Chicago, IL
Debater: Wassim Kassouf, MD, McGill University Health Center, Montreal, Quebec, Canada
Debater: Badrinath R. Konety, MD, Allina Health Center Institute, Minneapolis, MN
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023
References:
- Lamm DL, Blumenstein BA, Crissman JD, et al. Maintenance bacillus Calmette-Guerin immunotherapy for recurrent Ta, T1 and carcinoma in situ transitional cell carcinoma of the bladder: A randomized Southwest Oncology Group Study. J Urol. 2000 Apr;163(4):1124-1129.
- Oddens J, Brausi M, Sylvester R, et al. Final results of an EORTC-GU cancers group randomized study of maintenance bacillus Calmette-Guerin in intermediate- and high-risk Ta, T1 papillary carcinoma of the urinary bladder: one-third dose versus full dose and 1 year versus 3 years of maintenance. Eur Urol. 2013 Mar;63(3):462-472.
- Rentsch CA, Birkhauser FD, Biot C, et al. Bacillus Calmette-Guerin differences have an impact on clinical outcome in bladder cancer immunotherapy. Eur Urol 2014;66:677-688.
Optimizing BCG Therapy in Bladder Cancer: Expert Insights on Managing Toxicity and Maximizing Efficacy - Badrinath Konety & Wassim Kassouf


