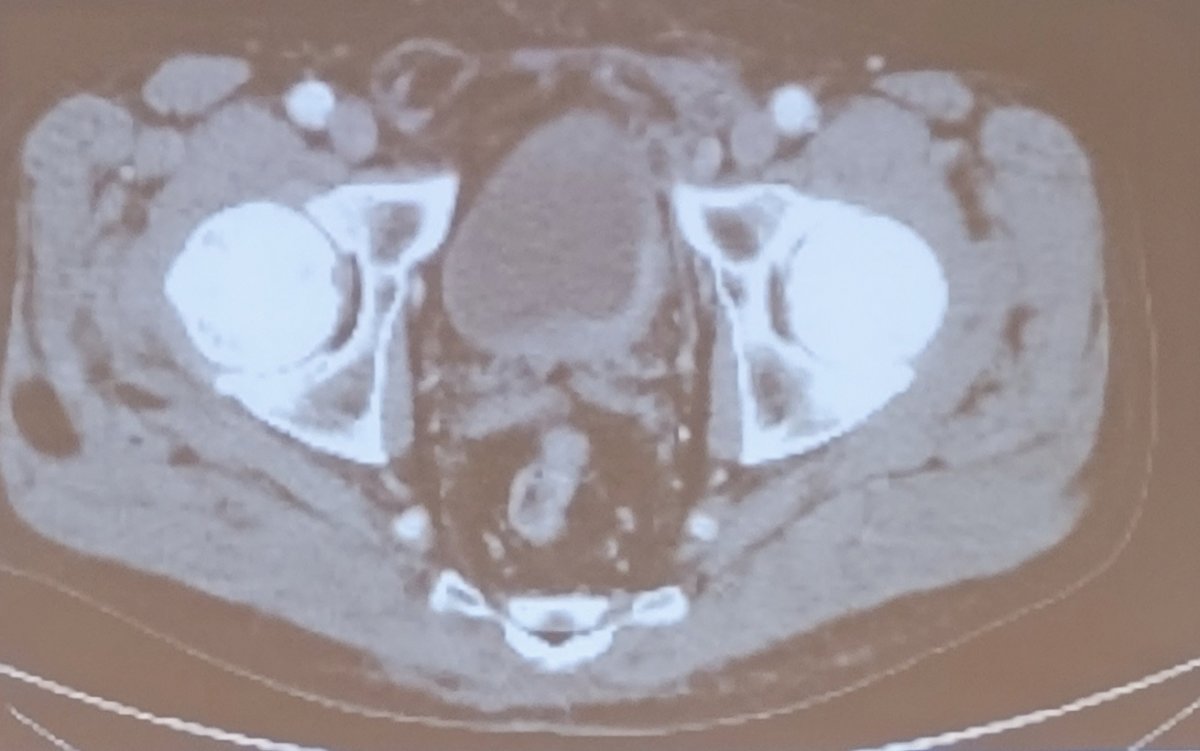
(UroToday.com) The 2023 AUA annual meeting included the Bladder Cancer Forum, featuring a debate discussing whether bladder preservation is a myth or reality in muscle invasive bladder cancer. Moderator Dr. Shilpa Gupta started her presentation with a case of a 75 year old man with hypertension, coronary artery disease s/p CABG x5, who presented with gross hematuria. A subsequent TURBT showed muscle-invasive bladder cancer, his ECOG PS was 1 and his creatinine clearance was 65 mL/min. He did have mild hearing loss and he wished to pursue bladder sparing options, if possible. The following is a representative image of his CT abdomen/pelvis showing focal thickening of the left posterior and lateral bladder wall, with no hydronephrosis and no lymphadenopathy:
Dr. Gupta then polled the audience asking “What would be your preferred treatment for this patient?”
- 30%: trimodality bladder preservation
- 52%: Neoadjuvant chemotherapy followed by radical cystectomy
- 13%: Neoadjuvant chemotherapy followed by trimodality bladder preservation
- 4%: Radical cystectomy alone
- 0%: Neoadjuvant immunotherapy followed by radical cystectomy
- 0%: Radical cystectomy followed by adjuvant immunotherapy
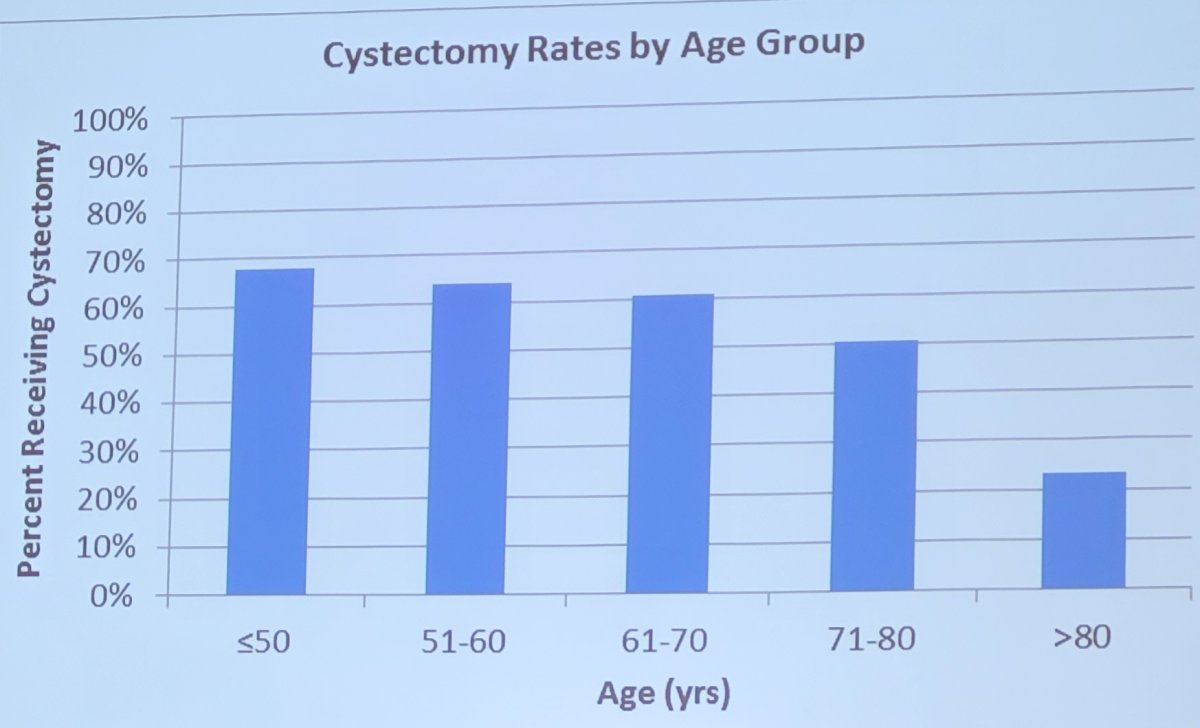
Dr. Jason Efstathiou then discussed the role of trimodality therapy for this patient. Dr. Efstathiou started by highlighting that trimodality therapy is a sheep in wolf’s clothing, representing a paradigm shift in contemporary oncology for organ preservation: (i) laryngeal carcinoma, (ii) anal carcinoma, (iii) breast carcinoma, (iv) esophageal carcinoma, and (v) limb sarcomas. The morbidity of radical cystectomy is not to be taken lightly, noting that among 1,142 radical cystectomies at MSKCC from 1995-2005, 64% of patients had more than one complication, 13% had grade 3-5 adverse events, 26% were readmitted, and 90-day mortality rate was 2.7%. Dr. Efstathiou also emphasized that radical cystectomy is not being performed in 50% of patients, thus there is a huge unmet need which trimodality therapy can fill the gap:
For the surgeons who think trimodality therapy may take away the surgical aspect of muscle invasive bladder cancer, Dr. Efstathiou notes that trimodality therapy is very much a surgical approach – in his mind, urologists are the quarterback for trimodality therapy as noted in the following algorithm (U denotes urologist):
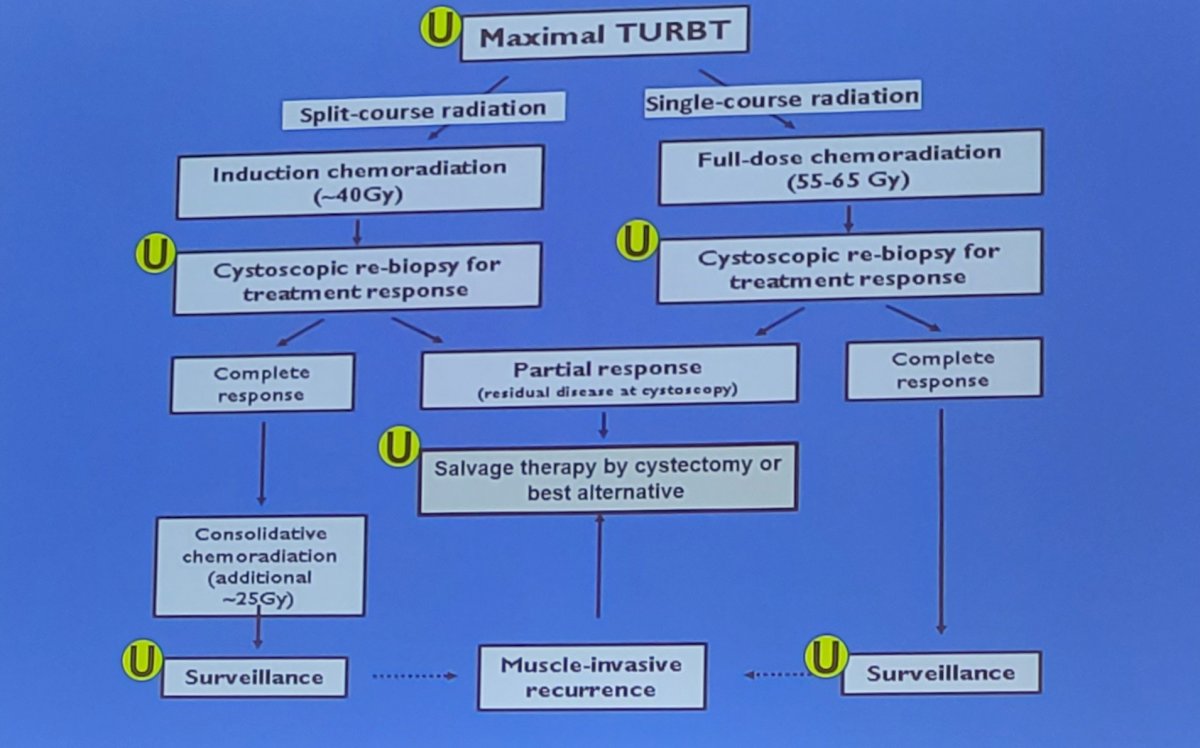
To support this, he notes that a quality/aggressive TURBT and salvage cystectomy (for the 10-15% that require it) is paramount to the success of trimodality therapy. At Massachusetts General Hospital, Dr. Efstathiou says that they have excellent long-term results with trimodality therapy that are comparable to radical cystectomy: among cT2 disease, 5-year DSS is 74% and 10-year DSS is 66%.1 Among patients treated in a contemporary setting (2005-2013), salvage cystectomy rates are only 15%.1 Dr. Efstathiou cautions that population-level database studies should be interpreted with extreme care, secondary to (i) patients unfit for surgery are not excluded, (ii) median radiotherapy fraction was 18 (typically >30 are needed for definitive therapy), (iii) confounding, misclassification, and selection bias are high.
According to Dr. Efstathiou, the most important study and compelling argument for trimodality therapy are from a multi-institutional (MGH, Toronto, USC), propensity score matched analysis (3:1) that is currently In Press at Lancet Oncology. Patients had to have solitary tumors <7 cm, no or only unilateral hydronephrosis, and no multifocal CIS. This study includes 1,116 patients (2005-2017) with muscle invasive bladder cancer that were included after matching (n = 834 radical cystectomy – median follow-up 4.38 years; n = 282 trimodality therapy – median follow-up 4.88 years), with a median age of 71, 75% male, 10% hydronephrosis, 60% underwent neoadjuvant chemotherapy, and 90% cT2. The 5-year metastasis free survival probability for trimodality therapy was 74% compared 74% for those undergoing radical cystectomy:
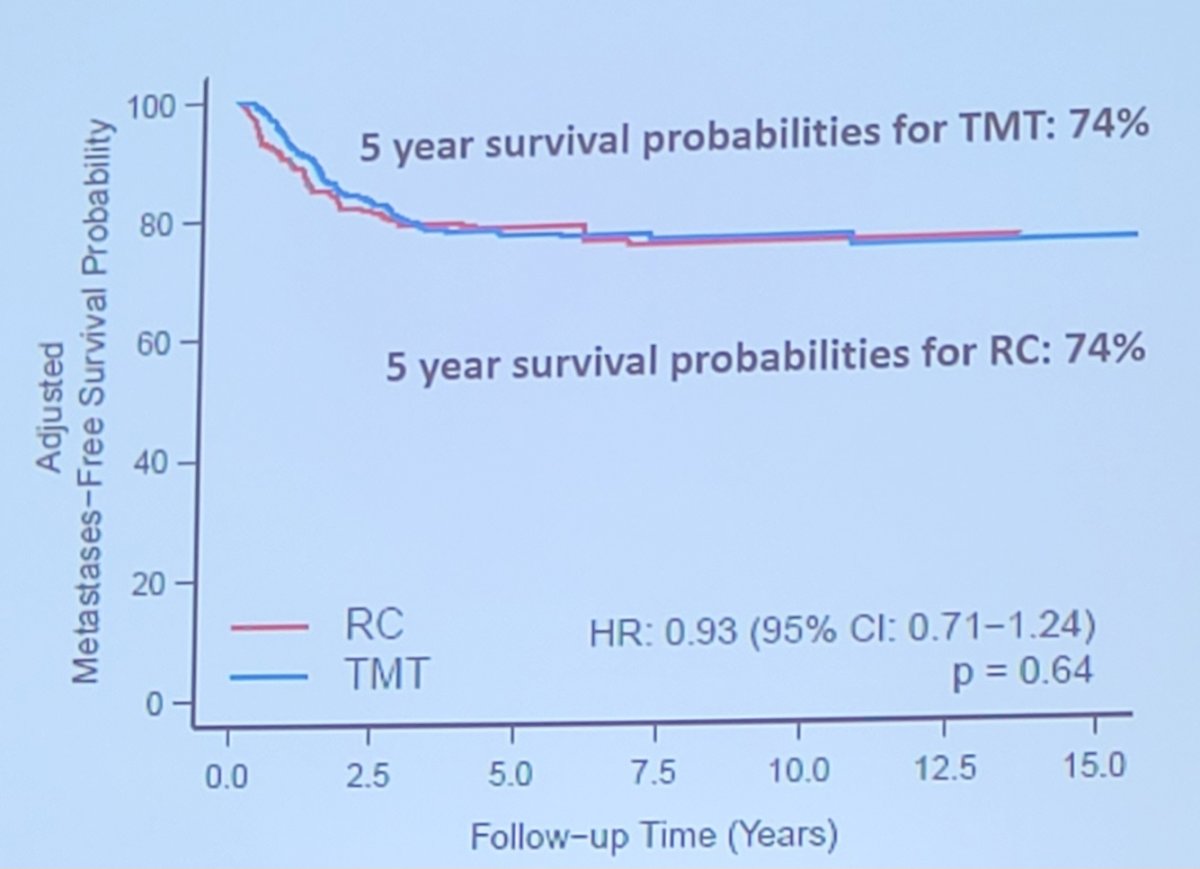
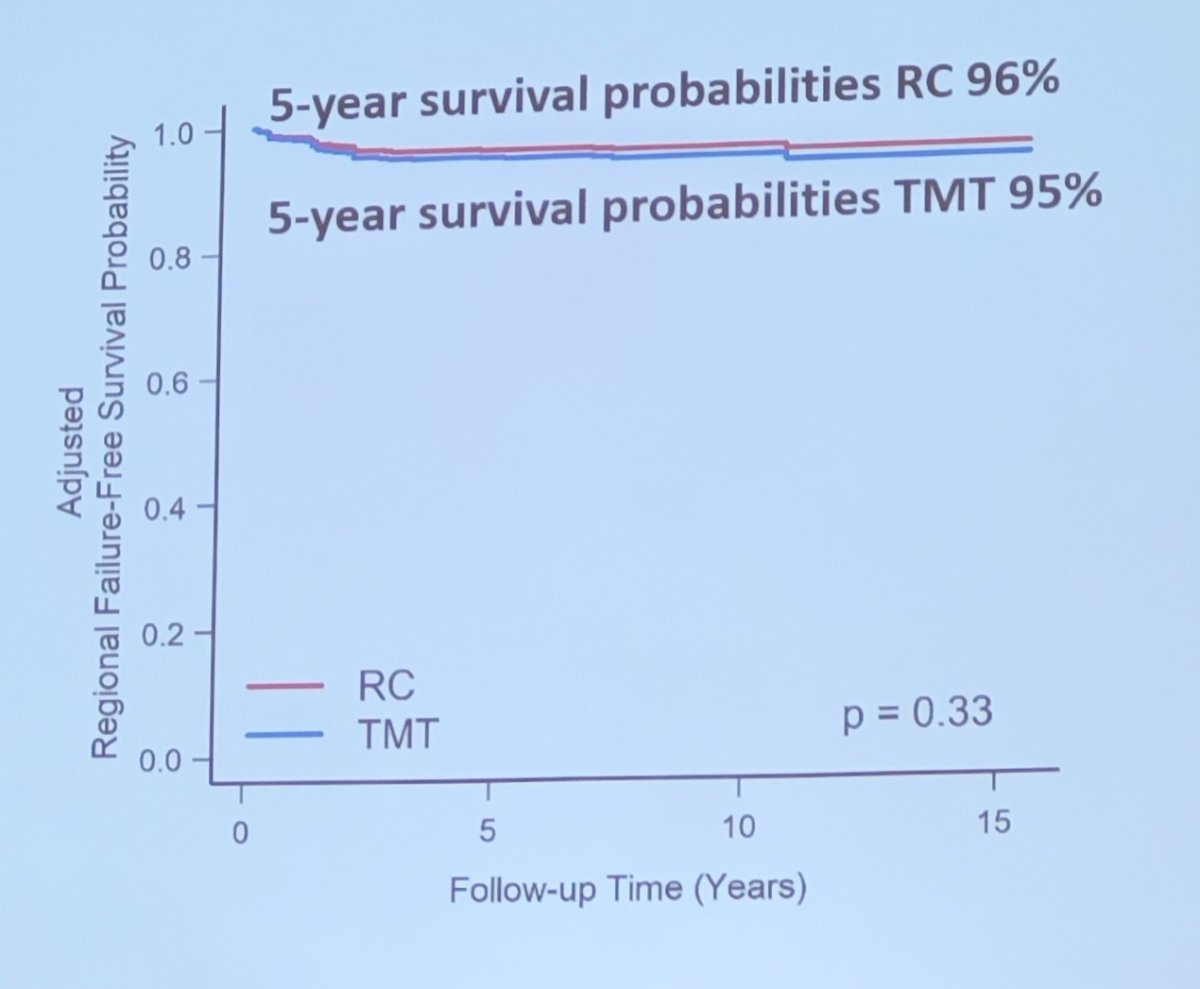
Similarly, there was no difference in 5-year regional failure-free survival between trimodality therapy (95%) and radical cystectomy (96%):
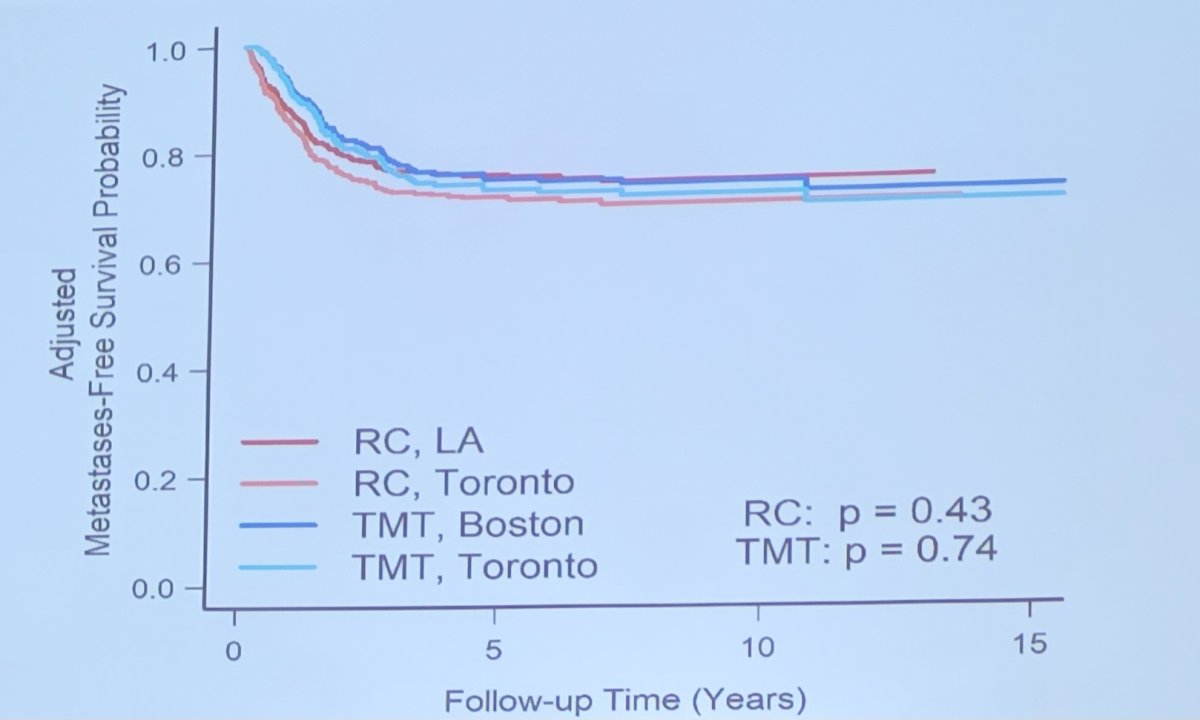
Importantly, there was no difference in metastasis free survival by treatment group and center, which suggests generalizability of trimodality therapy at centers of excellence:
Furthermore, in this study, salvage cystectomy was performed in 38 patients (13%) treated with trimodality therapy, and non-muscle invasive bladder cancer recurrence occurred in 57/278 (20.5%) of trimodality patients. Final pT stage in the whole cohort of 421 radical cystectomy patients was:
- pT0: 14%
- pT1: 7%
- pT2: 29%
- pT3/pT4: 42%
- N+: 24%
Peri-cystectomy mortality in the whole cohort of radical cystectomy patients (n = 421) was 2.5% and the median number of nodes removed in the surgical cohort was 39 nodes. Ultimately, 30% of muscle invasive bladder cancer patients who underwent radical cystectomy were also candidates were also candidates for trimodality therapy.
Long-term toxicity is acceptable and quality of life after bladder preservation is good (and probably better than after radical cystectomy). Late pelvic (GU or GI) grade 3+ toxicity from RTOG and BC2001 trials was 1-6%. Compared to radical cystectomy, trimodality therapy is associated with:
- Modestly higher general quality of life (by 7-10 points)
- Similar urinary scores
- Modestly higher bowel function (by 3-7 points)
- Markedly better sexual quality of life (by 9-32 points)
- Better informed decision making (by 14 points)
- Less concerns about appearance (by 14 points)
- Less life interference from cancer or cancer treatment (by 9 points)
Superficial recurrences can be managed conservatively, as 25% of patients will have non-muscle invasive tumors after complete response to trimodality therapy, including 60% recurrence free after TURBT and BCG. Salvage cystectomy is feasible for those that progress to muscle invasive bladder cancer and rates are ~15%. Dr. Efstathiou also highlights that trimodality therapy is noted as an option (alongside radical cystectomy) by the NCCN guidelines and is advocated for as an option by advocacy groups such as BCAN.
In a 2019 paper from Dr. Efstathiou’s group published in European Urology, there are initial studies supporting biomarkers that may predict who may benefit from trimodality therapy.2 This study found that signatures of T-cell activation and interferon gamma signaling were associated with improved DSS in a trimodality therapy cohort (HR 0.30, 95%CI 0.14-0.65), but not in the neoadjuvant chemotherapy and radical cystectomy cohort. Conversely, a stromal signature was associated with worse DSS in the neoadjuvant chemotherapy and radical cystectomy cohort, but not in the trimodality therapy cohort.
Finally, Dr. Efstathiou highlighted the INTACT SWOG/NRG 1806 Intergroup Phase III randomized clinical trial, which is randomizing patients with cT2-T4N0M0 bladder urothelial carcinoma to chemoradiotherapy vs chemoradiotherapy + 9 doses of atezolizumab
Dr. Efstathiou concluded his presentation emphasizing that in 2023, trimodality therapy should be offered to patients:
- Many muscle invasive bladder cancer patients are not getting any treatment, thus there is an undertreated and underserved population of patients
- 30% of surgical candidates are good trimodality therapy candidates plus all of the patients that are not surgical candidates
- Trimodality therapy is supported by numerous guidelines (NCCN, AUA/ASTRO/ASCO, EAU)
- In clinically matched patients, survival is comparable to radical cystectomy in the modern era
- >85% of contemporary patients keep their own bladder and long-term quality of life is good
- Trimodality therapy is not a non-surgical treatment, as maximal TURBT and salvage cystectomy are important components
- There are opportunities to continue to optimize clinical staging of the disease, delivery of radiotherapy and systemic therapies to improve outcomes
- Validation of biomarkers is necessary to guide bladder preservation therapy and for personalized treatment selection
Dr. Maria Ribal then discussed the argument that radical cystectomy is the best option for this patient. Dr. Ribal reiterated that trimodality therapy is only appropriate for very select patients (~20%). In the MCG institutional experience of trimodality therapy,1 she notes that the authors concluded that the data demonstrate long-term outcomes for trimodality therapy similar to radical cystectomy, and continue to support and establish the role for bladder-preserving trimodality therapy as an appropriate alternative to radical cystectomy for well-selected patients with muscle invasive disease who are motivated to preserve their native bladder. While there has been a randomized clinical trial showing superiority of trimodality therapy over bimodality therapy (TURBT followed by radiotherapy) for patients with muscle invasive bladder cancer, RCT evidence comparing trimodality therapy and radical cystectomy is currently neither available nor anticipated.
Williams et al.3 have also shown that trimodality therapy is more expensive than radical cystectomy. Among 2,963 patients included in this Medicare analysis, median costs were significantly higher for trimodality therapy than radical cystectomy in 90 days ($83 754 vs $68 692), 180 days ($187 162 vs $109 078), and 365 days ($289 142 vs $148 757), respectively:
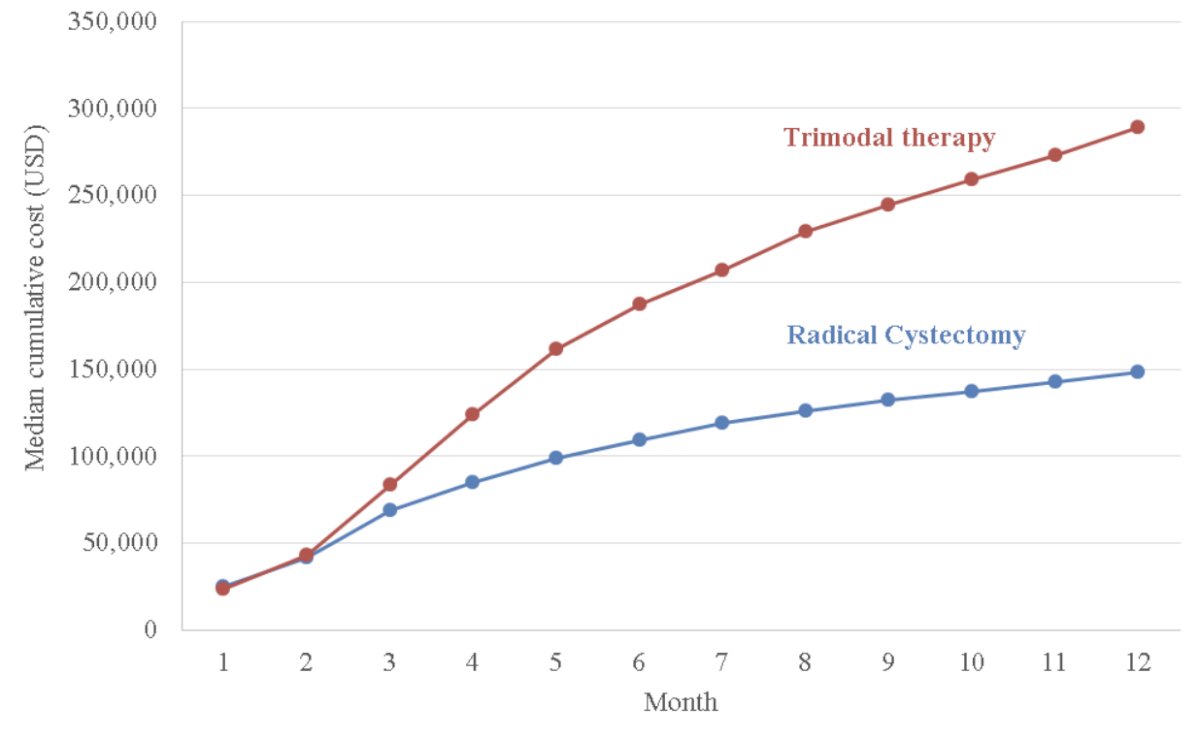
Outpatient care, radiology, medication expenses, and pathology/laboratory costs contributed largely to the higher costs associated with trimodal therapy. On inverse probability of treatment-weighted adjusted analyses, patients undergoing trimodal therapy had $136 935 (95% CI, $122 131-$152 115) higher mean costs compared with radical cystectomy 1 year after diagnosis.
So, how do we select patients? Previous studies have suggested that patients with cT3 disease have a ~58% increased risk for all cause mortality. With regards to age, Kumar et al4 found that in the US veteran population, for patients at least 65 years of age, treatment with trimodality therapy and a preferred chemotherapy was associated with similar overall and bladder cancer-specific mortality rates to those who underwent radical cystectomy and neoadjuvant chemotherapy. A worse overall mortality rate (HR 1.82) and bladder cancer specific mortality rate (HR 2.51) was found for patients younger than age 65 who received trimodality therapy and a preferred chemotherapy. As follows is a tabular summary highlighting bladder preservation patient selection criteria:

Dr. Ribal notes that complete and maximal TURBT is a key for trimodality therapy success. Additionally, 1/5 of patients treated with bladder sparing therapy with a curative intent will eventually require salvage radical cystectomy, which is associated with an increased risk of both complications and perioperative mortality.
Dr. Ribal concluded her presentation advocating for radical cystectomy with the following take-home messages:
- Although this patient is 75 years old, he has no comorbidities
- There is no data on CIS and on CT scan the tumor seems wider and is large
- Hearing loss could be a problem for chemotherapy
- Bladder function could be damaged, thus this patient would fare better with a radical cystectomy and ileal conduit
Moderator: Shilpa Gupta, MD, Cleveland Clinic Foundation, Cleveland, OH
Debater: Jason Efstathiou, MD, Massachusetts General Hospital, Boston, MA
Debater: Maria J. Ribal, Hospital Clinic, University of Barcelona, Barcelona, Spain
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023
References:
- Giacalone NJ, Shipley WU, Clayman RH, et al. Long-term outcomes after bladder-preserving tri-modality therapy for patients with muscle-invasive bladder cancer: An updated analysis of the Massachusetts General Hospital experience. Eur Urol. 2017;71:952-960.
- Efstathiou JA, Mouw KW, Gibb EA, et al. Impact of immune and stromal infiltration on outcomes following bladder-sparing trimodality therapy for muscle-invasive bladder cancer. Eur Urol 2019 Jul;76(1):59-68.
- Williams SB, Shan Y, Ray-Zack MD, et al. Comparison of costs of radical cystectomy vs trimodal therapy for patients with localized muscle-invasive bladder cancer. JAMA Surg. 2019 Aug 1;154(8):e191629.
- Kumar A, Cherry DR, Courtney PT, et al. Outcomes for muscle-invasive bladder cancer with radical cystectomy or trimodal therapy in US veterans. Eur Urol Open Sci. 2021 Jun 9;30:1-10.


