(UroToday.com) During his presentation, Dr. Brian Shuch from UCLA Medical School discussed the importance of considering renal cancer histologic subtypes when designing treatment plans. He is a member of experts in developing NCCN guidelines for the treatment of kidney cancer.
To begin, he provided a concise overview of the epidemiology of kidney cancer. He highlighted that the incidence of renal cell carcinoma (RCC) has risen by 2.5 times in the past thirty years, potentially due to advances in imaging technology. Additionally, there may be a correlation between the increase in RCC rates, obesity, and longer life expectancies.
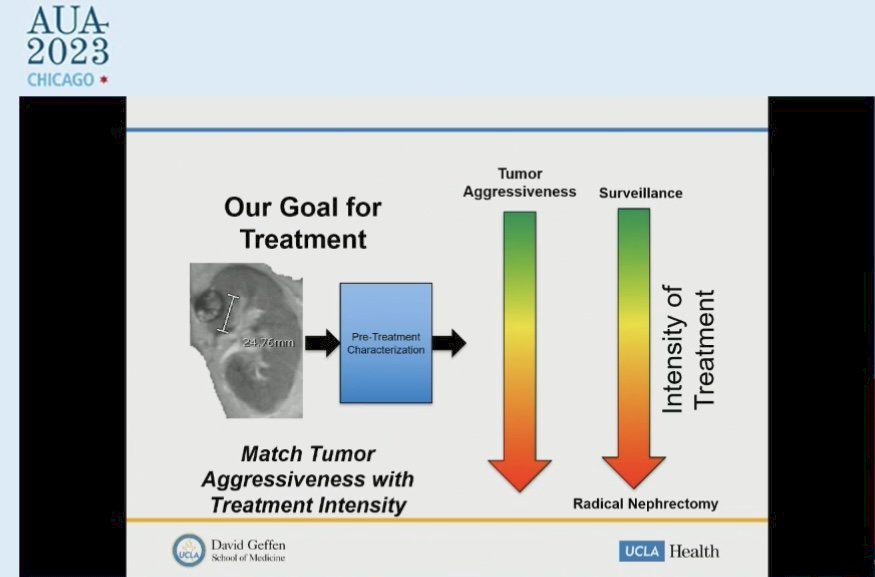
While current guidelines for selecting a treatment plan for kidney cancer rely on tumor size, it's important to note that size alone may not provide a complete picture. It's also crucial to consider the aggressiveness of the tumor when making treatment decisions. Therefore, taking both size and aggressiveness into account can improve the accuracy and effectiveness of treatment planning.
Dr. Shuch touched upon common benign renal tumors, including papillary adenoma less than 1.5 cm, renomedullary interstitial cell tumor, which is being found in 40% of autopsies, oncocytomas, AML including fat-poor variants, metanephric adenomas, and mixed epithelial and stromal tumors (MEST).
Then, he mentioned emerging renal tumor entities including but not limited to biphasic hyalinizing psamomatous (BHP), biphasic squamoid alveolar (BSA), papillary renal neoplasm with reverse polarity (KRAS), warthin-like papillary RCC, thyroid-like follicular RCC, and eosinophilic vacuolated tumor (“High-grade oncocytic”).
Even for T1 Renal masses, the subtype impacts aggressiveness. Each cancer has different invasive and metastatic potential, and nuclear grade is not validated for all histology variants.
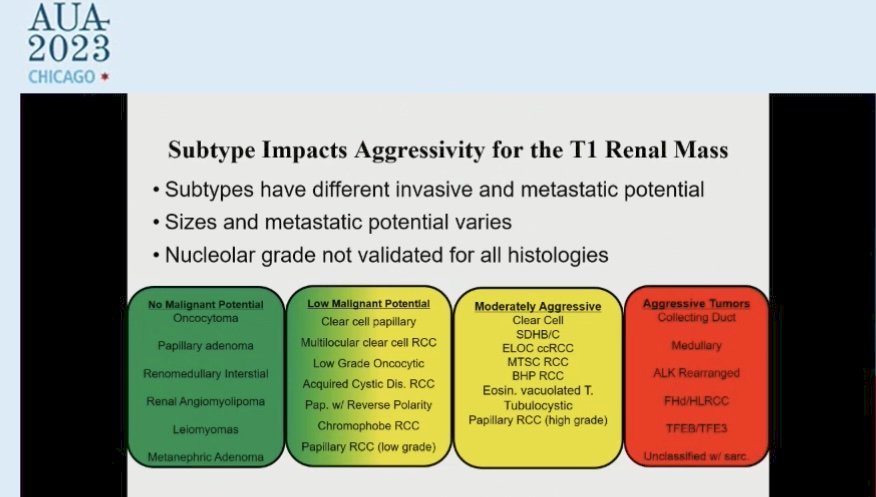
Although the histologic feature is not included in the management of small renal tumors, they almost never cause harm, and indolent histology can always have safe initial monitoring.
Then Dr. Shuch reviewed the outcomes of the management of renal tumors.

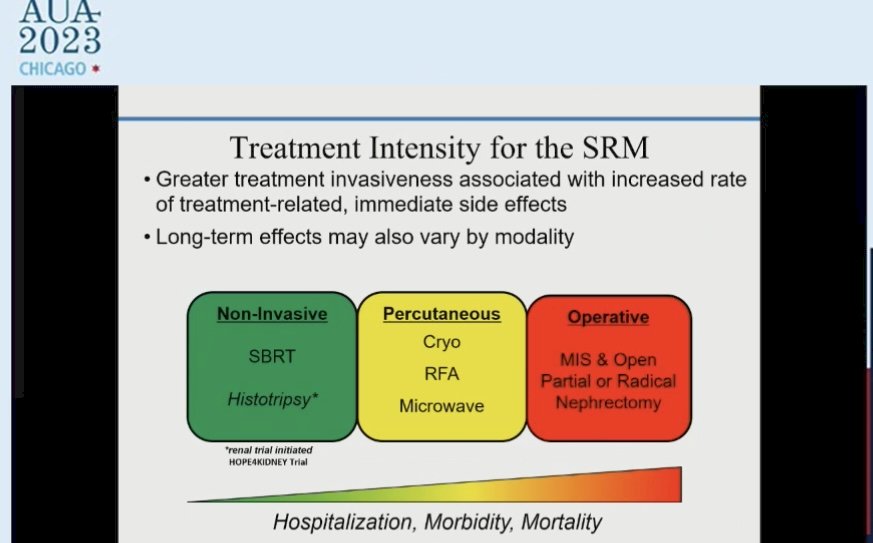
Research indicates that non-surgical complications can lead to mortality in 1 out of every 300 patients who undergo surgical treatment for renal cancer within 90 days of the procedure. Furthermore, increasing treatment intensity for small renal tumors is associated with higher rates of hospitalization, morbidity, and mortality. These findings suggest the importance of carefully considering the risks and benefits of different treatment approaches for kidney cancer patients.
Thanks to advances in imaging modalities, immunohistochemistry (IHC), and gene sequencing, histology identification has become possible in 2023 for kidney cancer patients. Renal mass biopsy, for example, has demonstrated high accuracy, with a positive predictive value (PPV) of 97.5% and a negative predictive value (NPV) of 82.5% for renal cell carcinoma (RCC). Several reliable IHC biomarkers have also been identified to aid in diagnosis. However, it's important to note that the best results are achieved through close collaboration with an expert GU (genitourinary) pathologist.

Multi-phased imaging, such as T2-weighted imaging and Sestamibi scans, have shown promise in predicting the histologic features of kidney masses. For instance, T2-weighted imaging has an 85% specificity for papillary tumors, while Sestamibi scans reveal high mitochondrial content, a feature commonly seen in chromophobe RCC and renal oncocytoma. Additionally, 89Zr-TLX-250 PET/CT has the potential to aid in detecting clear cell RCC.
In his closing remarks, Dr. Shuch emphasized the importance of the "RCC community GOALS" to prevent adverse events in the management of renal mass. He identified several keys that urologists should strive to avoid, including performing radical nephrectomy on a small benign renal mass, performing partial nephrectomy on an indolent tumor in elderly patients, using incomplete ablation for an aggressive renal mass larger than 4 cm, and performing elective partial nephrectomy in elderly patients at high risk of local recurrence. It emphasizes the importance of the RCC community goals and how they can ultimately benefit patients by improving outcomes and minimizing harm.
Presented by: Brian Shuch, MD, Associate Professor of Urology, Director, Kidney Cancer Program. UCLA School of Medicine, Los Angeles, CA, USA
Written by: Seyed Hossein Hosseini Sharifi, MD, Department of Urology, University of California Irvine, @Sharifi_shh on Twitter during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023


