(UroToday.com) The 2023 AUA annual meeting included a uroradiology session, featuring a presentation by Dr. Simon Soerensen discussing a comparison of an artificial intelligence model versus radiologists for the detection of clinically significant prostate cancer on MRI. Indeed, automated detection of prostate cancer on MRI may help target biopsies and avoid unnecessary biopsies of false-positive lesions. As such, Dr. Soerensen and colleagues sought to develop an artificial intelligence model to rapidly and accurately identify cancer foci on MRI and compare its performance against radiologists.
For this study, there were 1,504 subjects that underwent multiparametric MRI at more than 30 institutions in the US, followed by MRI-ultrasound fusion biopsy at one institution. The investigators used T2-weighted images (T2WI), apparent diffusion coefficient maps (ADC), and diffusion-weighted imaging (DWI) from 1,404 cases to train an artificial intelligence model. MRI lesions were initially identified and outlined by a radiologist using T2WIs, DWIs, ADC, and contrast enhanced images (DCE), and prostate cancers were confirmed by biopsy. Only lesions containing Gleason 3+3 (≥ 40% cancer core length) or Gleason ≥3+4 (any amount) in at least one targeted biopsy core were considered for training and testing the model; all other MRI lesions were removed. Systematic cores with significant cancer were also included for model training. Dr. Soerensen also tested the artificial intelligence model on 100 independent cases and compared it against trained radiologists. The artificial intelligence (U-Net) architecture for the detection of cancerous lesions on MRI is as follows:

Additionally, they computed lesion-level AUC, sensitivity, specificity, and negative predictive value.
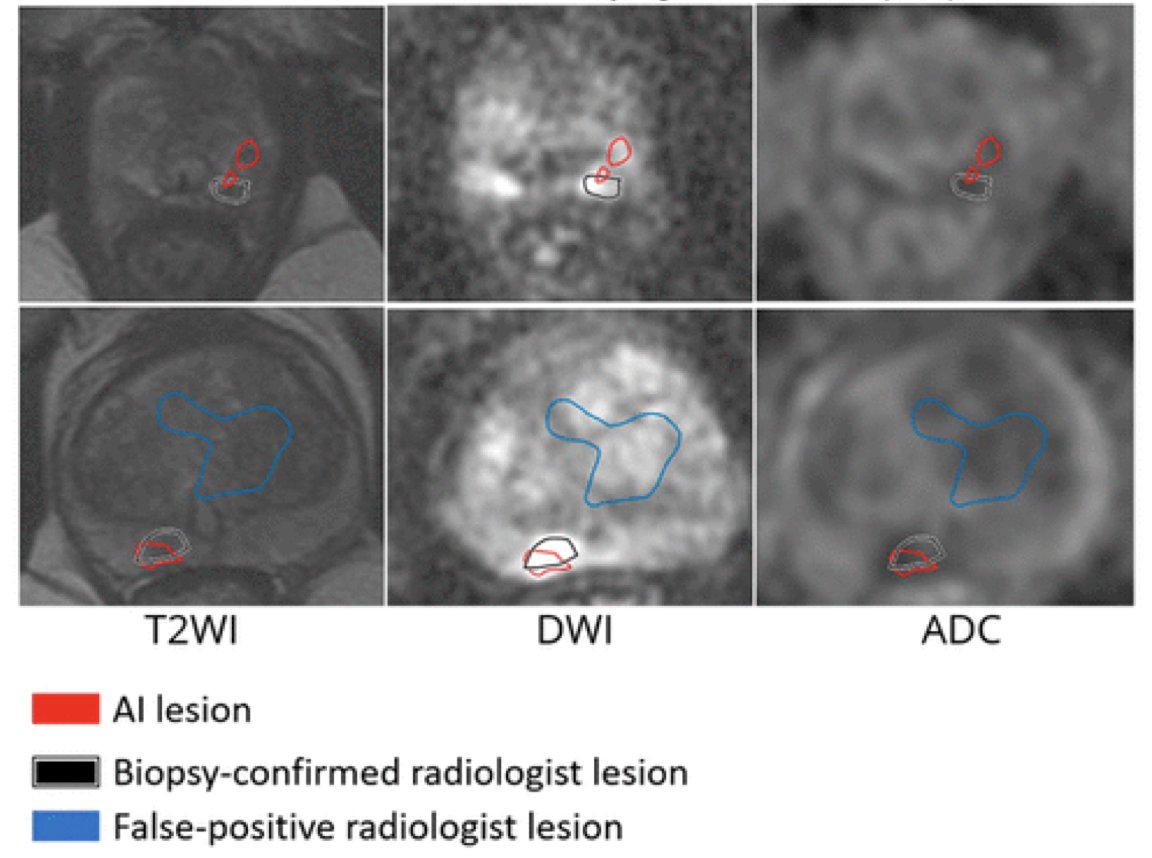
Artificial intelligence and radiologists had similar performances across all metrics, and all differences were non-significant. At the lesion level, the artificial intelligence model had an AUC of 0.76 ± 0.29, negative predictive value of 0.98 ± 0.09, sensitivity of 0.74 ± 0.43, and specificity of 0.85 ± 0.20. At the lesion level, radiologists had an AUC of 0.81 ± 0.24, negative predictive value of 0.98 ± 0.10, sensitivity of 0.76 ± 0.43, and specificity of 0.86 ± 0.15. As follows is two MRI slices of a representative case; T2WI, ADC, and DWI are overlaid with biopsy-confirmed radiologist lesions (black), AI predictions (red), and radiologist lesions that turned out to not contain clinically significant cancer (blue):
Dr. Soerensen concluded his presentation by discussing a comparison of an artificial intelligence model versus radiologists for the detection of clinically significant prostate cancer on MRI with the following take-home messages:
- In this study, an artificial intelligence model was trained and tested on a large and diverse multi-institutional cohort of MRIs
- The model matched the performance of radiologist experts
- In future work, Dr. Soerensen and colleagues envision comparing model performance against radiologists at different skill levels, comparing radiologist + artificial intelligence vs radiologist performance alone, and implement the model prospectively
Presented by: Simon J. C. Soerensen, MD, Stanford University, Paolo Alto, CA
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023


