(UroToday.com) The 2023 American Urological Association (AUA) annual meeting held in Chicago, IL between April 28 and May 1st, 2023, was host to an advanced prostate cancer podium session. Dr. Stephen Freedland presented the results of a real-world study examining outcomes among men with non-metastatic castration-sensitive biochemical recurrence after definitive therapy and with short PSA doubling times receiving early secondary treatment.
Dr. Freedland highlighted that there is no consensus for the treatment of men with non-metastatic castrate sensitive prostate cancer (nmCSPC) with biochemical recurrence (BCR) after definitive treatment with radical prostatectomy or radiotherapy. While the impact of PSADT on prostate cancer outcomes after BCR is well-established for patients receiving delayed ADT, the natural history of treated BCR and the role of PSADT in early treated prostate cancer remains less clear. Factors that predict the future development of metastatic disease have been proposed to guide treatment decisions and include:
- Timing of initial PSA elevation
- Gleason Score
- PSADT
The objective of this study was to assess real-world outcomes in men with nmCSPC and short PSADT who experienced BCR following definitive treatment, as compared to men with longer PSADT and historical controls.
In this study, the investigators reviewed the Veterans Health Administration (VHA) database between January 2006 and June 2020 to identify men with nmCSPC and BCR post-definitive treatment. Men had a PSADT of 15 months or less and were categorized into rapid (≤9 months) and less rapid (9-15 months) PSADT groups. Study outcomes included time to first antineoplastic treatment after BCR and MFS. Cox proportional hazards models were used to compare the two PSADT cohorts, adjusting for baseline demographics and clinical characteristics.
This study included a total of 781 patients as demonstrated in the study flow chart below: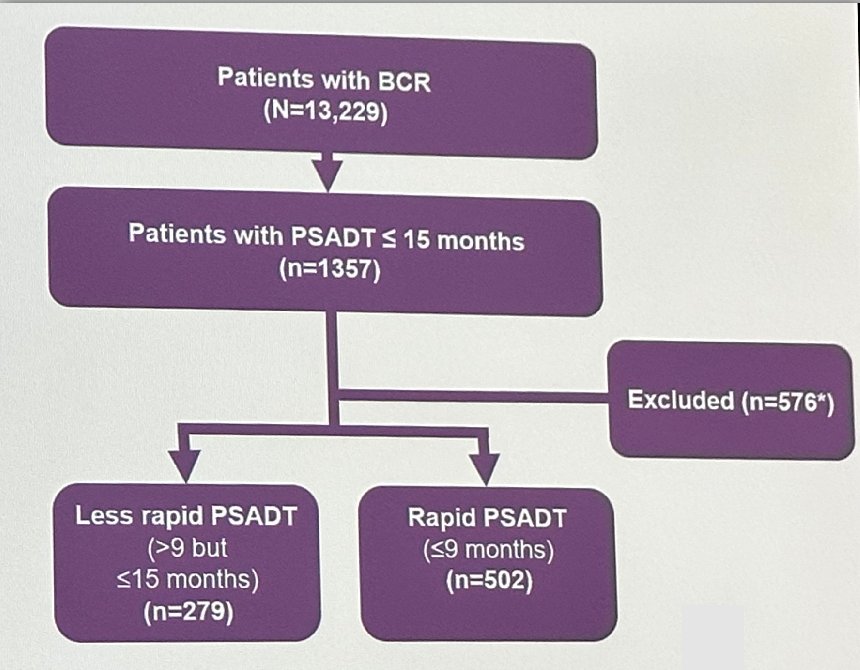
With regards to baseline characteristics, patients in the rapid PSADT cohort had a significantly shorter time from definitive treatment to index (32.3 versus 48.5 months, p<0.05). PSA level at index was comparable between the two groups.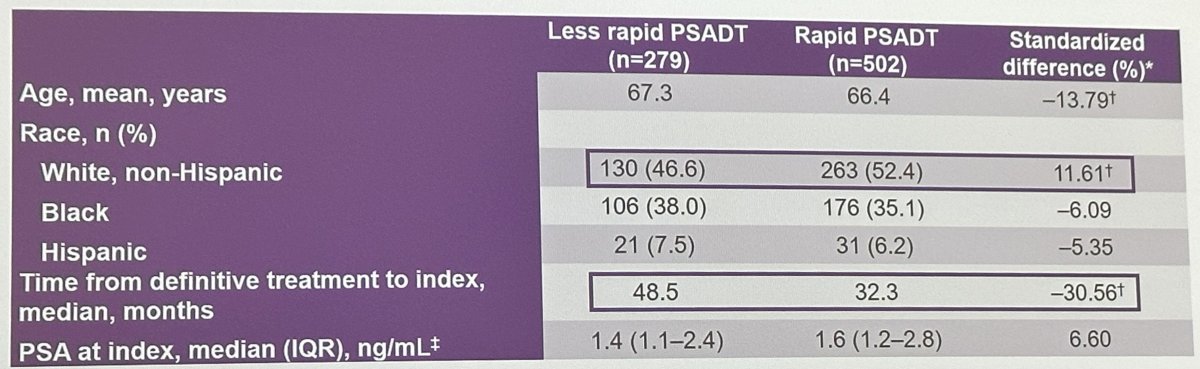
First regimens received after BCR were comparable between the two cohorts: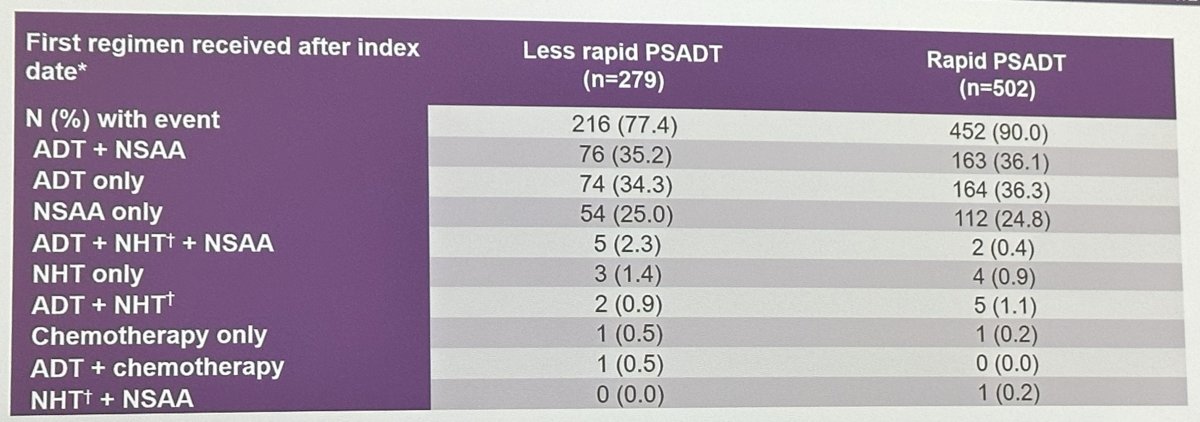
At a median follow-up time of 56 months, the time to first antineoplastic treatment after BCR among nmCSPC patients was significantly shorter in the rapid PSADT cohort (median 11.4 versus 28.3 months; aHR: 2.09, 95% CI: 1.76-2.48).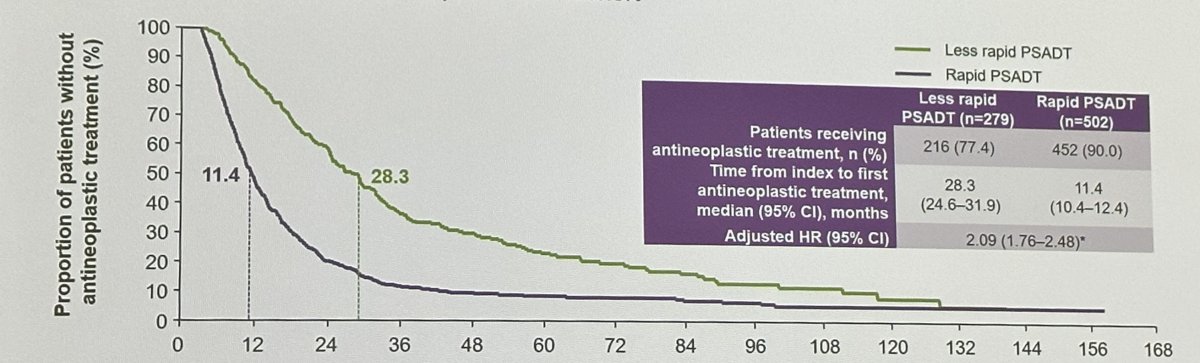
Similarly, MFS outcomes were significantly worse in the rapid PSADT cohort (aHR: 1.79, 95% CI: 1.33 – 2.40).
Of note, the median MFS in men with rapid PSADT closely approximated the median MFS for all patients with BCR after radical prostatectomy in the reported cohort by Pound et al.1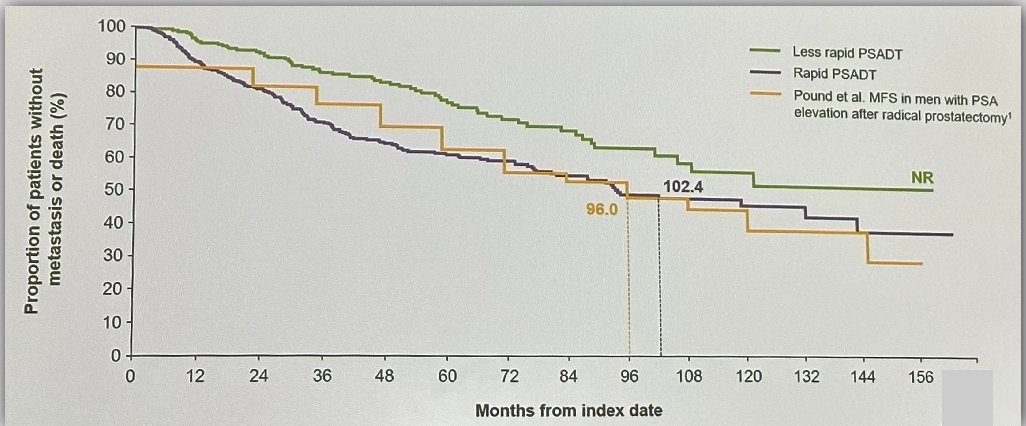
No significant differences in OS were observed between the two PSADT cohorts. However, outcomes in both groups were superior to those observed by Freedland et al. in 2007,2 which is likely a reflection of the increased availability of life-prolonging therapies in this disease space.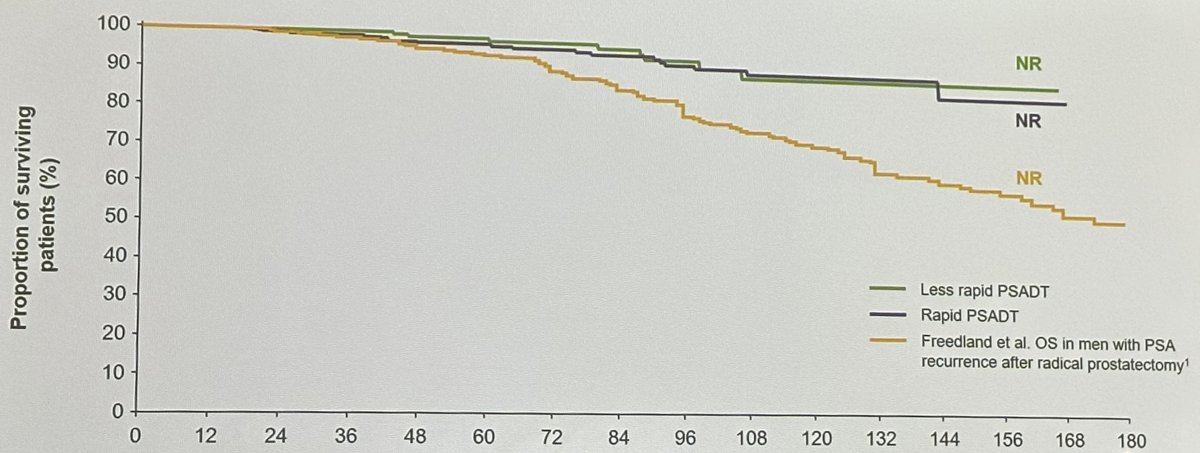
Dr. Freedland concluded his presentation as follows:
- Most rapid PSADT men (≤9 months) underwent secondary treatment within 1 year of BCR, compared with less rapid PSADT men (53% versus 18%), whereas most of the less rapid PSADT men remained treatment-free for >2 years
- Median MFS in men with rapid PSADT was 102.4 months, closely approximating the Pound data from Hopkins, wherein median time to metastases after BCR was 96 months (8 years)
- However, the Pound data included all BCR patients, not just those with rapid PSADT
- Also in the Pound data, no patients received early hormonal treatment, whereas most VHA patients received secondary treatment within 1 year of BCR
- While circumstantial, the fact that rapid PSADT VHA patients heavily treated with secondary treatment options had similar outcomes to all BCR patients in the Pound series, where none received aggressive secondary treatment, suggests the potential benefit of aggressive early treatment of men with rapid PSADT after BCR
- OS after BCR among nmCSPC patients in this study was better than was previously reported for men with BCR after radical prostatectomy in the cohort study by Freedland et al.
Presented by: Stephen Freedland, MD, Professor, Department of Urology, Cedars Sinai Hospital, Los Angeles, CA
Written by: Rashid K. Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023
References:
- Pound CR, et al. Natural history of progression after PSA elevation following radical prostatectomy. JAMA, 1999.
- Freedland, et al. Death in patients with recurrent prostate cancer after radical prostatectomy: prostate-specific antigen doubling time subgroups and their associated contributions to all-cause mortality. J Clin Oncol, 2007.


