(UroToday.com) The 2023 American Urological Association (AUA) annual meeting held in Chicago, IL between April 28 and May 1st, 2023, was host to the British Association of Urological Surgeons/BJU International/Urological Society of Australia and New Zealand (BAUS/BJUI/USANZ) session. Drs. Sigrid Carlsson, Hashim Ahmed, and Renu Eapen discussed whether PSA screening is a proactive measure or simply a counterproductive test for our patients.
PSA screening - Proactive
Dr. Carlsson opened the floor trying to make an argument in favor of PSA screening. She explained prostate cancer (PCa) is the second most frequent cancer and the fifth leading cause of cancer-related death among men in the world, and its incidence is steadily growing. The incidence of PCa in the world in 2025 is estimated to be 1.8 million, with 500,000 estimated cancer-related deaths. Most men will develop prostate cancer if they live long enough. It is estimated that in US white men 80+ years-old, 47% will be found to have PCa at autopsy, and 51% of US black men will have prostate cancer between 70-79 years of age.
Despite all efforts to improve treatment-related toxicity, the patient reported outcomes in the ProtecT trial have shown that the rates of urinary incontinence, sexual dysfunction, and bowel dysfunction after treatment for PCa are still high, and Dr. Carlsson, argued that sometimes “doing less could be more” if we want to avoid harming our patients. Active surveillance (AS) is the preferred management option for low-risk localized PCa in 2023. It is endorsed by multiple practice guidelines including the AUA/ASTRO/SUO, FAU-ESTRO-ESUR-SIOG, ASCO, NCCN, and NICE. AS is widely adopted around the world, and it is increasingly becoming a treatment option in select men with grade group (GG) 2 PCa. In the US, the use of AS among men with low-risk PCa is increasing, and in 2021 almost 60% of low-risk PCa patients were treated with AS.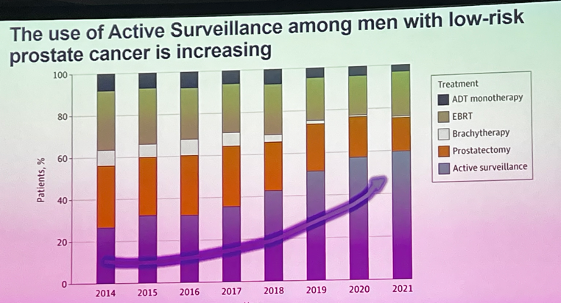
The Memorial Sloan Kettering Cancer Centre (MSKCC) published in 2020 their experience with AS. They reported on 2,664 men with GG1 and 219 men with GG2 disease. With a median follow-up of 4.3 years, only 1 patient died of PCa and 5 patients developed metastasis, confirming AS is a safe management strategy for appropriately selected and monitored men.
In the most recent years, we have seen a definitive and sustained increase in PCa metastases in the US, which is consistent with decreases in PSA screening, based on previous USPSTF recommendations.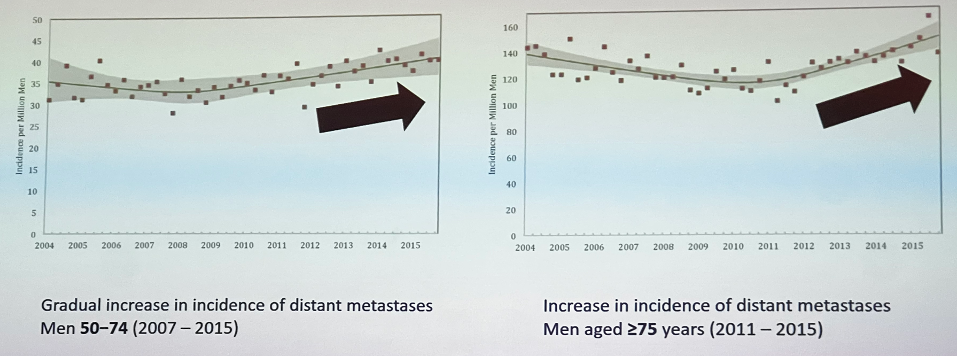
Dr. Carlsson explained that the death rate from PCa in the US declined from the mid-90s through 2010, but has stabilized in recent years, possibly due to the gradual increase in incidence of metastatic disease. See the image below.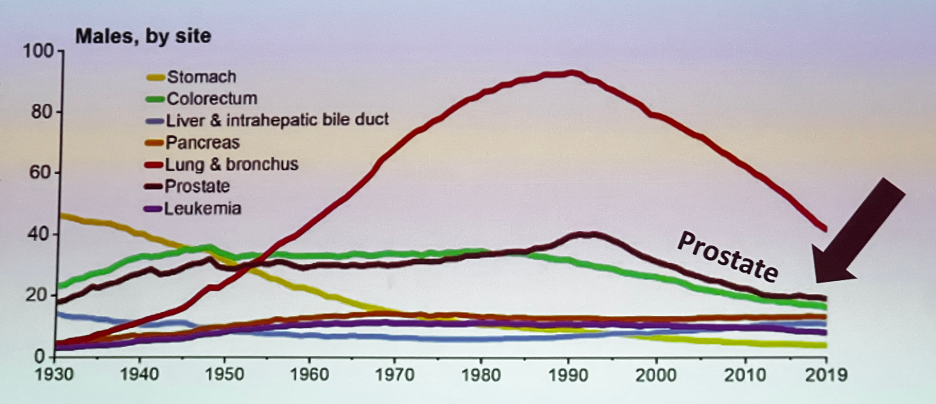
The recently published Early Detection of Prostate Cancer: AUA/SUO Guideline 2023 recommends using PSA as the first screening test for PCa early detection. Dr. Carlsson explained that at the time of evidence review for this guideline, very limited evidence was available regarding other candidates than PSA for first-line biomarkers or imaging.
PSA-level in midlife strongly stratifies long-term risk of distant metastasis or death from PCa. The PSA-level at age 60 is a powerful predictor of 25-year risk of lethal PCa. 90% of PCa deaths occurred in men with PSA in the top quartile (PSA ≥ 2ng/mL), and men with PSA below median (≤ 1.0 ng/mL) at age 60, are unlikely to die from PCa (0.2% risk).
PCa screening has evolved from DRE only screening in 1984 when 30-35% of patients were diagnosed with bone metastatic disease, to widely use PSA screening, after its introduction in 1987. PCa screening trials in the US (PLCO) and Europe (ERSPC) have reported data of 76,000 and 182,000 patients, respectively. These trials initially favored the discontinuation of PSA screening, as they showed no clear benefit in reducing PCa-specific mortality with a PSA screening strategy. With re-evaluation of the screening trials, it has been reported that the control arm in the PLCO study had contamination, and up to 90% of the individuals had at least one PSA test during their follow-up. Moreover, confirmation by analytic microsimulation models showed reduction of PCa-mortality in the PLCO and ERSPC trials.1
Dr. Carlsson continued to discuss the PRAISE-U project. This project aims to reduce morbidity and mortality caused by PCa in EU Member States through smart early detection and direct partnership with a network of consortium members, using customized and risk-based screening programs that are patient-tailored and that use a risk-based approach. PRAISE-U will be the hub in combining science with implementation for early detection of PCa. The recently published paper by Professor Van Poppel proposing a risk-stratified early detection strategy was presented and is shown in the image below.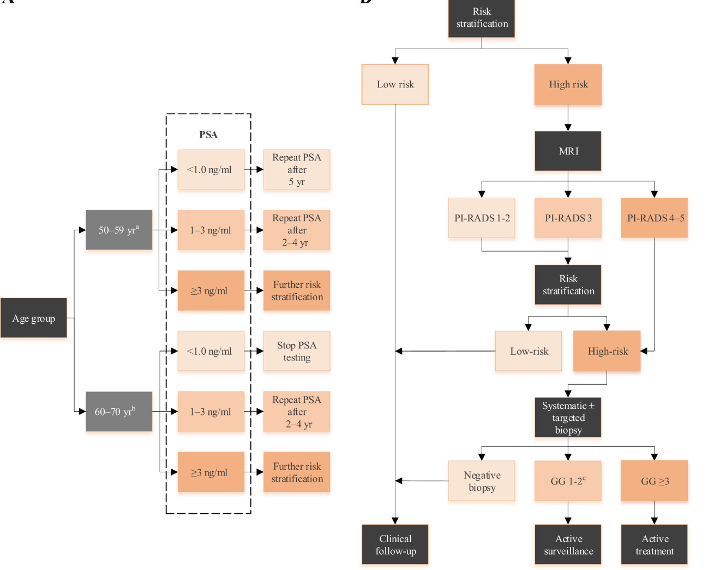
Dr. Carlsson discussed the ongoing Swedish regional organized PCa testing programs (OPT), for which now 17 regional programs have been launched and by next year 17 of 21 Swedish regions would have OPT programs. Furthermore, multinational published and ongoing PCa screening trials were discussed, in which multiple diagnostic modalities (MRI, molecular testing) are being used for PCa screening. Summary in the below image.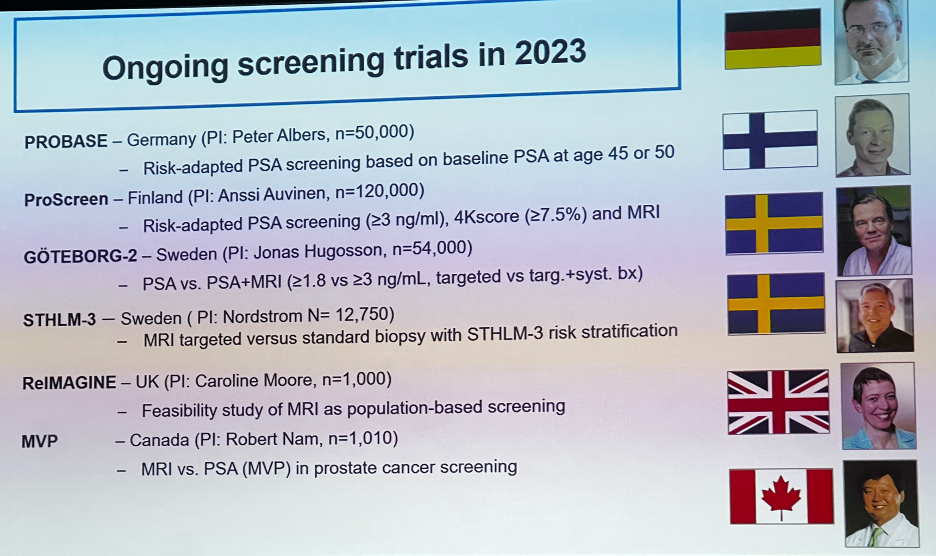
The PROBASE trial was discussed. This is an ongoing randomized trial of risk-adapted screening for PCa comparing patients starting at age 45 versus 50 years. The investigators have recruited 23,301 patients in the first round of the trial, and reported that the prevalence of screen detected PCa in 45-year-old patients was very low (0.02%), and only 4 patients have been diagnosed with aggressive (≥ GG3) PCa.
The STHLM3 test is a multiplex test that combines clinical information (age, family history, prior biopsy), blood biomarkers (total PSA, free PSA, ratio of free to total PSA, hK2, MIC-1, and MSMB), and genetics. The STHLM3 test has a higher predictive accuracy compared to PSA alone (AUC 0.74 versus 0.56). Dr. Carlsson presented the data from the STHLM3-MRI trial which compared different screening strategies that used combinations of risk prediction, MRI-targeted biopsy, and systematic biopsy in a population-based, organized, screening-by-invitation design. This trial confirmed that performing targeted and systematic biopsies, only in men with positive MRI, prevented unnecessary biopsies, decreased over-detection, and maintained the number of clinically significant cancers found. See image below.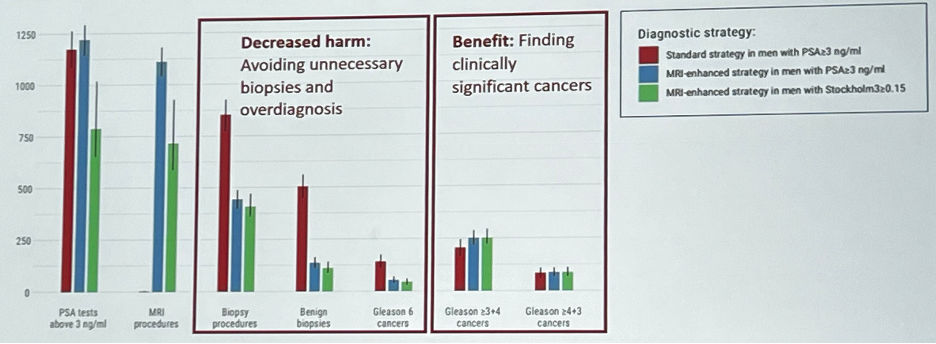
Dr. Carlsson summarized the GOTEBORG-2 trial, this trial examined if omitting systematic biopsy for all men with an elevated PSA (≥3 ng/mL) and performing targeted biopsy of only MRI-positive lesions could reduce the risk of detecting clinically insignificant prostate cancer, but at the same time maintaining the detection of clinically significant cancer. A 0.7% reduction in diagnosing clinically insignificant cancer was reported (RR 0.45, p<0.001), and no difference in the detection of clinically significant disease was found.
Dr. Carlsson concluded her talk by saying that PSA screening is proactive if done well.
PSA screening - Counterproductive
Professor Hashim Ahmed made an argument for why PSA screening is counterproductive. He discussed the Wilson and Junger screening criteria and based his talk on whether a PSA screening strategy for PCa meets these criteria. See image below.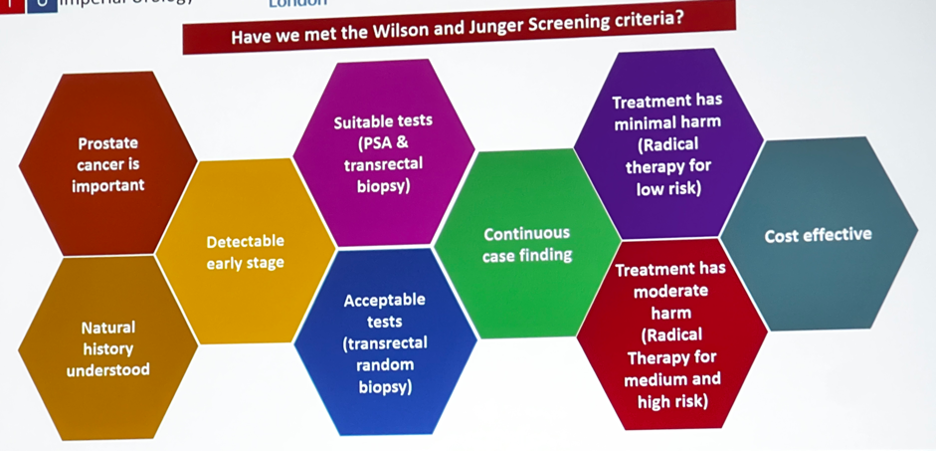
He went on to explain why the mortality benefit conferred by screening for PCa using PSA testing followed by transrectal systematic biopsy is at best uncertain. Data from the CAP randomized clinical trial and the PLCO screening trial were presented. He reported that population-based data of PSA screening has shown no mortality benefit and that the extended follow-up of the PLCO trial showed a higher number of diagnoses of clinically insignificant PCa.
Data from the ERSPC trial showed that the number needed to invite, and the number needed to diagnose to prevent one death from PCa were 570 and 18 individuals, respectively. This PSA screening trial also showed a higher probability of diagnosing clinically insignificant PCa and conferred PSA a low sensitivity (57%) and specificity (82%) for detecting clinically significant disease.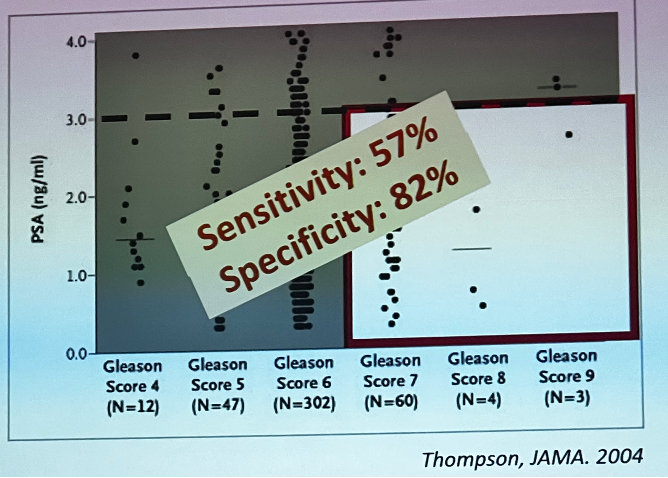
Professor Ahmed made a point on why transrectal systematic, or as he prefers to call it “random” biopsy, is inaccurate, harmful and he believes is holding back the cause of screening. MRI is still underutilized in 2023, with 60% of men not having an MRI prior to a biopsy in the US; If used, most men are still undergoing systematic biopsies and not benefiting from the triage role of pre-biopsy MRI. Prof. Ahmed suggested that rather than dealing with the underlying issue of overdiagnosis and overtreatment of PCa by improving screening and diagnostic methods, instead, we are trying to wage this issue on the pathologists by advocating to stop calling GG1 'cancer'.
MRI usually misses very few clinically significant PCa cases. Data from a post-hoc analysis of PROMIS and PICTURE trials showed how MRI mostly detects clinically significant disease and avoid detection of GG1 PCa. See image below.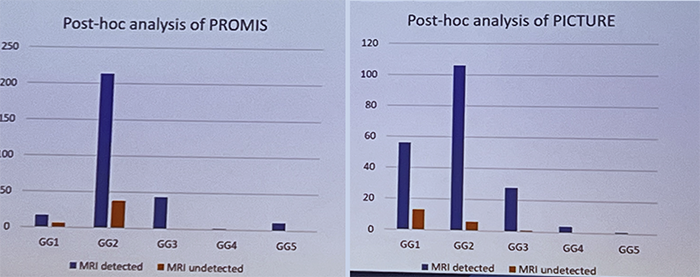
Professor Ahmed discussed the Regional application of MRI pre-biopsy (RAPID) programme in the U.K. The RAPID pathway required patients with an MRI score 4 or 5, and those with an MRI score of 3 and a PSA density ≥0.12, to undergo a biopsy. This program allowed 43% of men to avoid a prostate biopsy while preserving good detection of clinically significant cancers, and low detection of insignificant cancers. See figure below.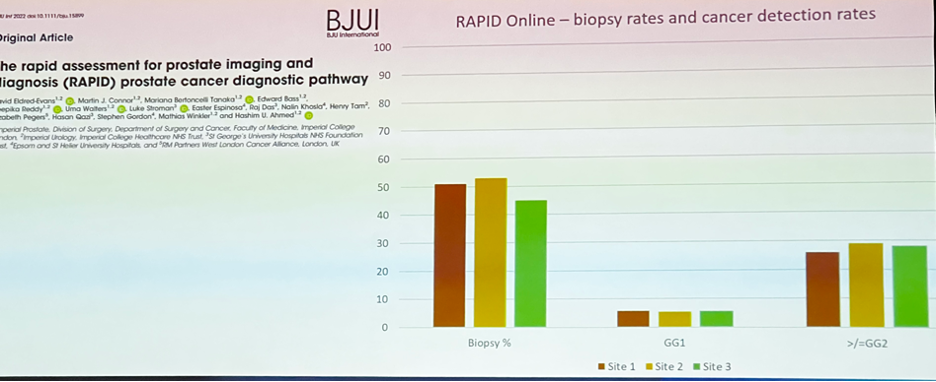
The discussion shifted towards MRI becoming a screening test for PCa. Prof. Ahmed made the point, that despite making MRI a first-line screening test for PCa. We must take into consideration the current MRI capacity in the world, and the overwhelming financial commitment from governments to use MRI as a screening test. He argued that we may not be there yet.
Professor Ahmed presented the data from the 15-years outcomes of the ProtecT trial and showed there is no difference in PCa-specific mortality regardless of the treatment of choice in low and intermediate-risk PCa patients. He went on to discuss the recently presented data of the PACE-A trial which compared SBRT to surgery for localized PCa. Despite the improvement in surgical techniques and surgical technologies, robotic radical prostatectomy is still associated with a 47% pad use at 2 years according to this trial. See image below.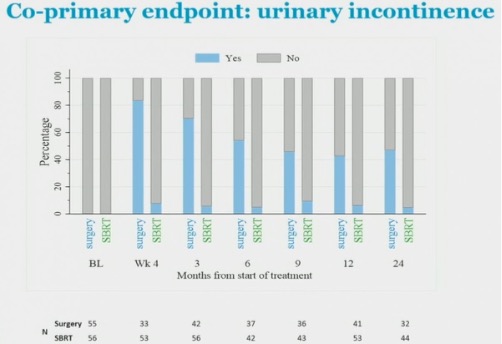
Professor Ahmed discussed that once PCa is diagnosed the harms of treatment are high and likely underestimated; rates of AS, AS burden, and transition to radical therapy are still disappointing in 2023. Despite AS being increasingly used, 40% of men still get radical treatment if diagnosed with low-risk PCa in the US. He advocated that harm reduction therapies such as focal therapy are not offered routinely, and they should be. He presented data on how urinary issues, incontinence, and impotence are far more common with radiotherapy or radical surgery when compared with focal therapy, with similar survival rates at 5-10 years.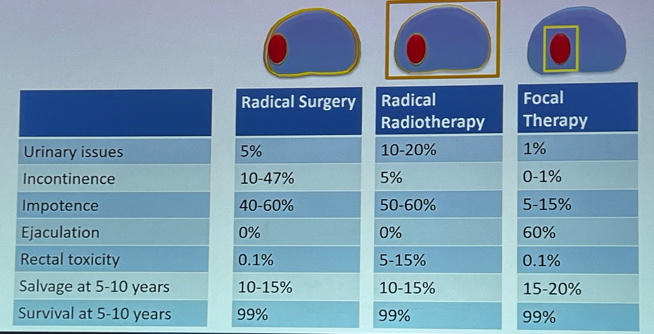
Professor Ahmed concluded his talk saying that despite all efforts, we have not met the Wilson and Junger screening criteria (there is lack of suitable and acceptable tests for screening, treatment has a high probability of harming the patient, and PSA screening for PCa is not cost effective). Dr. Ahmed concluded that we can’t justify screening at this point with PSA, therefore, PSA screening is counterproductive.
PSA Screening – The Australian Perspective
Dr. Renu Eapen presented the PSA screening and early diagnosis Australian perspective. A summary of how PCa screening has changed for the last 13 years was presented. In 2010 there was widespread use of PSA, DRE, no patient counselling, and our diagnostic method was sextant blind TRUS biopsy of the prostate. Inevitably, this led to overdiagnosis and overtreatment of many patients. In 2023 we now offered Informed consent and shared decision making about PSA screening, we still use PSA (and DRE), but also newer tools for risk stratification (PHI, PCA3, 4K score), mpMRI, and in Australia they have mostly switched to doing transperineal (TP) and targeted biopsy exclusively.
There has been a PCa grade migration phenomenon in Australia, with studies demonstrating grade migration towards diagnosis of higher grade PCa. Partly driven by changes in PSA testing recommendations, improved diagnostic pathways with multiparametric MRI, switch from TRUS to MRI targeted and systematic TP biopsies, and the use of PSMA PET in improving diagnosis of clinically significant PCa in Australian clinical trials.
Dr. Eapen presented data on the largest registry of PCa in Australia and New Zealand. This is the Prostate cancer outcomes registry sponsored by Movember. The PCO registry has gathered data from 250 sites across Australia and NZ, with >91,000 people enrolled, and 382 clinicians involved. The registry has shown that TP biopsies are becoming the preferred method for diagnosis of PCa, and the rates of active surveillance for low-risk disease are steadily increasing from 2015 to 2019. See image below.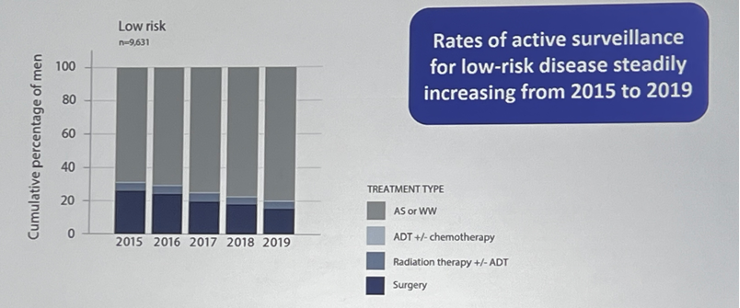
Dr. Eapen discussed the results of the recently published PCOR-VIC study which reported the decade-long trends in PCa biopsy grade groups, and treatment within a population-based registry. This study showed how the number of TP biopsies increased from 16% in 2013-2014 to 90% in 2019-2020 in Australia. With the shift towards TP biopsies, a reduction in diagnosing GG1 disease was observed, and an increase in clinically significant PCa was also documented, arguably, because of a better targeting of suspicious lesions with transperineal biopsy. There was also a substantial decline in GG1 disease treated by surgery or radiotherapy, and GG discordance between biopsy and final pathology: was higher for TRUS (43%) vs TP biopsy (33%).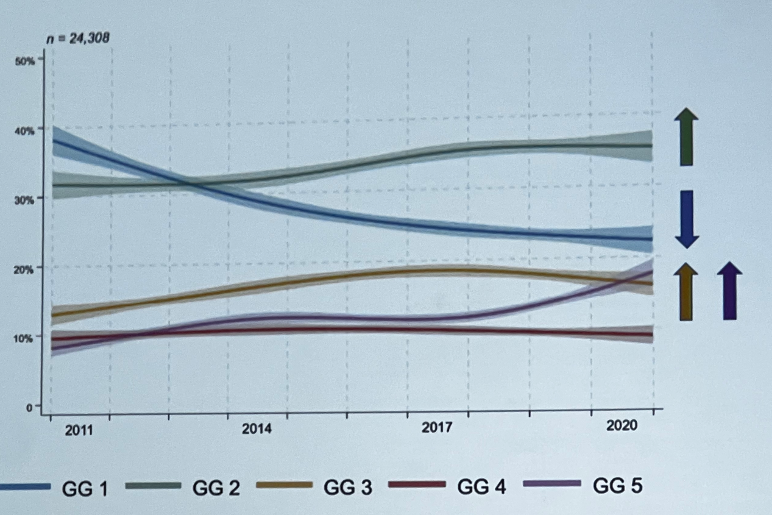
The PRIMARY imaging trial was discussed. This is a prospective multi-centre study that included 296 men with suspected PCa with a recent MRI (<6 months) who had an indication for prostate biopsy and underwent a PSMA PET/CT. The study showed a higher sensitivity and NPV when MRI and PSMA PET were combined, suggesting that they have a complementary role. Additionally, in ancillary analysis the SUVmax was found to be a good predictor of clinically significant PCa. When the SUVmax was >9 and the MRI was positive (PI-RADS 4-5) the PPV was 100%, and if the SUVmax was greater than 12 (any MRI result) the PPV was 100%. Finally, Dr. Eapen presented the ongoing phase II PRIMARY 2 trial, which is currently evaluating the addition value of PSMA PET in men with negative or equivocal MRI to diagnose clinically significant PCa.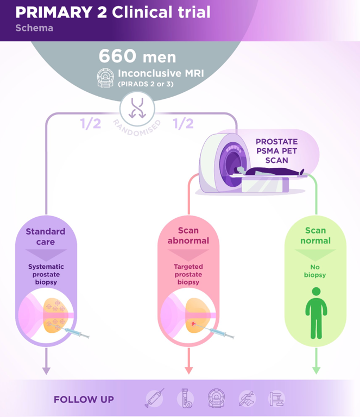
Dr. Renu Eapen wrapped up her presentation delivering strong key take away messages:
- PSA is still our best biomarker.
- Understanding limitations of PSA is critical.
- Adequate patient counseling, shared decision making should be incorporated into our practice.
- There is still work to do to solve the problems of overdiagnosis and overtreatment of PCa.
- PSMA PET may have a future role in detecting csPCa.
- We should minimize risks of PSA screening with best practice management.
- Sigrid Carlsson, MD, PhD, MPH, Director of Clinical Research, Josie Robertson Surgery Center; Assistant Attending Epidemiologist, Memorial Sloan Kettering Cancer Center, New York, NY
- Professor Hashim U. Ahmed, BM BCh (Oxon), Professor and Chair of Urology, Imperial College London, London, UK
- Renu Eapen, MBBS, FRACS (Urol), Department of Urology, Peter MacCallum Cancer Centre, Melbourne, Australia
Written by: Julian Chavarriaga, MD – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @chavarriagaj on Twitter during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023
Related Content:
Improving Primary Prostate Cancer Diagnosis Through Risk Stratified Screening: a European Perspective - Sigrid Carlsson


