(UroToday.com) The 2023 American Urological Association (AUA) annual meeting held in Chicago, IL between April 28 and May 1st, 2023, was host to the International Prostate Forum, with Dr. Jeffrey Karnes discussing the role of metastasis-directed therapy for patients with oligometastatic, hormone-sensitive prostate cancer.
Oligometastatic prostate cancer is often seen as an intermediary state in the progression from organ-confined to widely metastatic disease, although some have argued that the oligometastatic state is a non-intermediary, biologically/clinically unique state with distinct molecular signatures, not along the metastatic disease continuum. There is no consensus volume definition, with cut-offs ranging from 1 to 5, typically defined per conventional imaging.
The concept of oligometastasis in prostate cancer is not a novel one. In 1988, Soloway et al., stratified patients with metastatic prostate cancer based on extent of disease on the initial bone scan. 166 men were stratified based on the number of bone scan-detected metastases, with increasing number of lesions associated with worse survival outcomes:
- Group 1: >6 metastatic lesions
- Group 2: 6 – 20
- Group 3: >20
- Group 4: Superscan
Why treat oligometastases in such patients? Treatment of the oligometastatic lesions may actually help induce/mediate control of the primary tumor. Targeting of the oligometastases lesions may also improve response to systemic therapy by reducing the mutational load, eradicating the immunosuppressive state, and improve the efficacy of ADT, while also removing persistent sources of future metastases,
Is there a rationale for local treatment of patients with oligometastatic disease? HORRAD was a multicenter prospective RCT of 432 patients with previously untreated, de novo mHSPC at 28 centers across The Netherlands between November 2004 and September 2014. All eligible patients had a PSA >20 ng/ml and documented bone metastases on bone scan. Patients were randomized in a 1:1 fashion to either ADT with EBRT or ADT alone, with a primary endpoint was OS. The median PSA was 142 ng/mL and over a median follow up of 47 months, the median OS was non-significantly different at 45 months in the radiotherapy + ADT arm compared to 43 months in ADT alone arm (HR 0.90, 95% CI 0.70 to 1.14).2
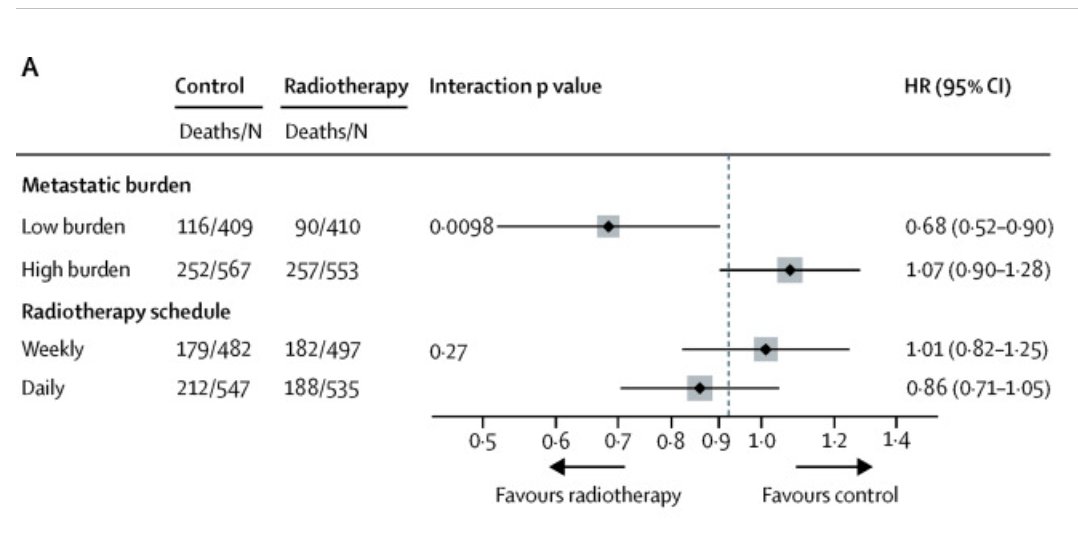
STAMPEDE (Arm H) was an open label, randomized controlled phase III trial of 2,061 men. This arm randomized patients with de novo mHSPC in a 1:1 fashion to standard of care + radiotherapy or standard of care alone between January 2013 and September 2016. Standard of care was defined as lifelong ADT with upfront docetaxel permitted from December 2015 onwards. Men allocated to radiotherapy received either a daily (55 Gy/20fx) or weekly (36 Gy/6fx). This trial demonstrated OS benefits in the CHAARTED low volume group only (HR 0.68, 95% CI 0.52 to 0.90), with no significant benefits observed in the overall or high-volume groups.3
We await results from PEACE-1 and SWOG 1802, both evaluating systemic therapy plus definitive therapy (PEACE-1: RT only, SWOG 1802: RT or RP) versus systemic therapy alone, which will be available in the upcoming few years.
What about the use of radical prostatectomy (RP) for such patients? Dr. Karnes referenced the study by Mason et al. published in The Journal of Clinical Oncology in 2015. This trial randomized patients with cT3-4N0/xM0 prostate cancer or cT1-2 + PSA >40 or 20-40 + GS 8-10 to either lifelong ADT alone or ADT + RT. At a median follow-up of 8 years, overall survival was significantly improved in the patients allocated to ADT+RT (HR; 0.70; 95% CI: 0.57 – 0.85, p<0.001).4 As such, Dr. Karnes argued that such results with a HR of 0.70 should set the bar for future RP studies in this setting.
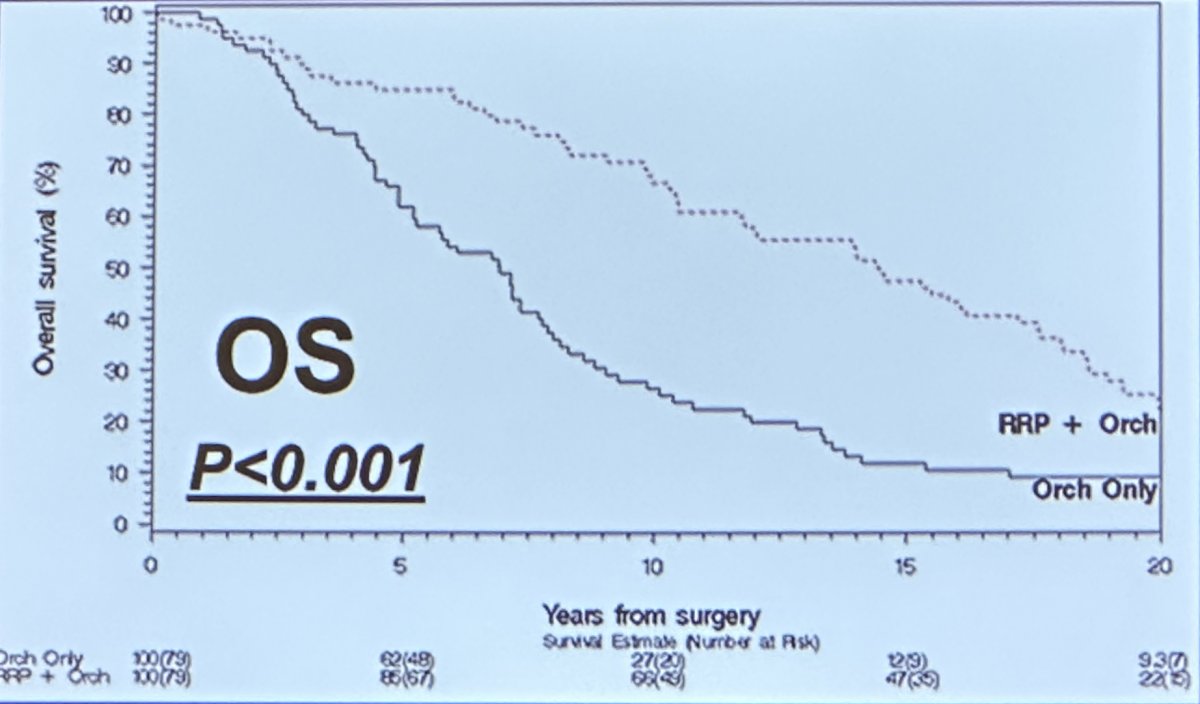
In 1999, Ghavamian et al. published the results of a retrospective, matched cohort analysis of patients undergoing an orchiectomy only (n=79) versus an RP + orchiectomy (n=79) between 1966 and 1995. The 10-year overall survival was noted to be significantly longer in the RP + orchiectomy group (65% versus 30%).5
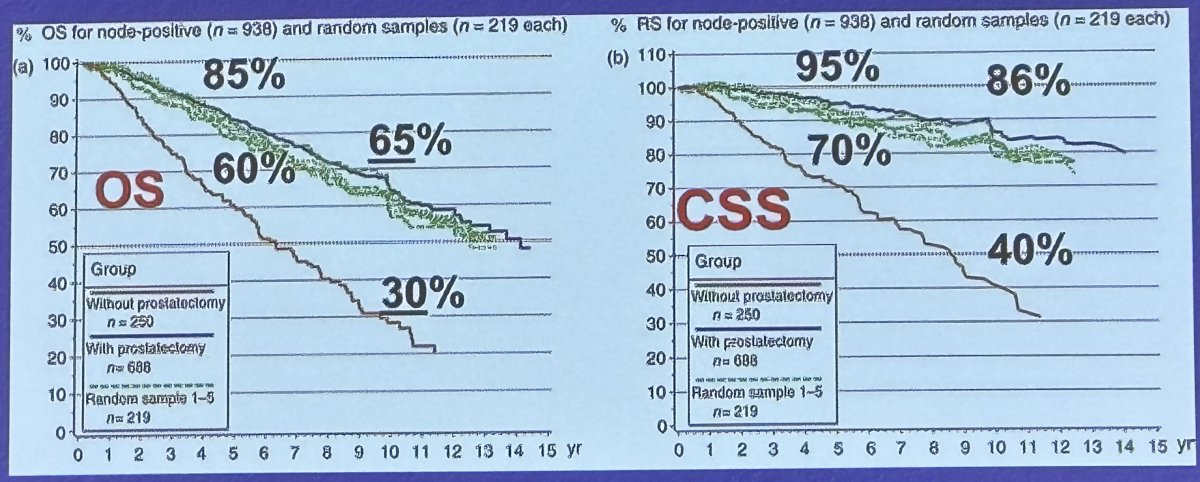
Analysis of the Munich Cancer Registry published in 2010 demonstrated that RP had significant OS and CSS benefits in patients with pathologic nodal positive disease, with the authors arguing as such that RP should not abandon in node-positive cases.6
Dr. Karnes argued that there are clues from ECOG 3886 (positive trial) and EORTC 3084 (negative trial) of immediate versus delayed hormonal therapy to suggest that RP may be beneficial for patients with pN+ disease. Patients in the positive ECOG 3886 trial had an RP performed, whereas those in the negative EORTC 30846 trial did not. This was reflected in 10-year overall survivals of 65% and ~30% in ECOG 3886 and EORTC 30846. As such, these findings may to some degree be secondary to patients in the ECOG 3886 trial having underwent an RP.7,8
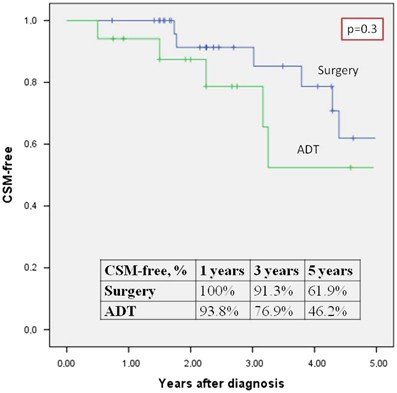
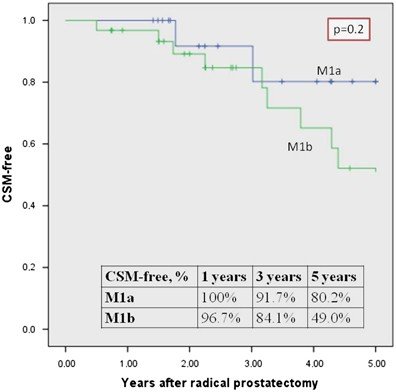
In 2017, Dr. Karnes’ group reported on the outcomes of 47 patients with M1a-b disease, 31 of whom underwent a radical prostatectomy at The Mayo Clinic (remaining 16 received ADT alone). 5-year cancer-specific survival rates were 62% in the RP group, compared to 46% in the ADT only group (p=0.3). Outcomes were also non-significantly different between M1a and M1b patients.9
Retrospective case series in this disease space (prostate cancer with bone metastases) have demonstrated inconsistent benefits for RP.

Ongoing trials in this disease space include:
- SWOG 1802 which is randomizing patients with metastatic prostate cancer to best supportive therapy +/- definitive therapy (RT or RP)
- 660/1270 patients have been enrolled
- Now allows for PSMA PET and MDT (if done prior to randomization)
- TRoMbone study (<3 m1b)
- 50 patients randomized to SOC +/- RP
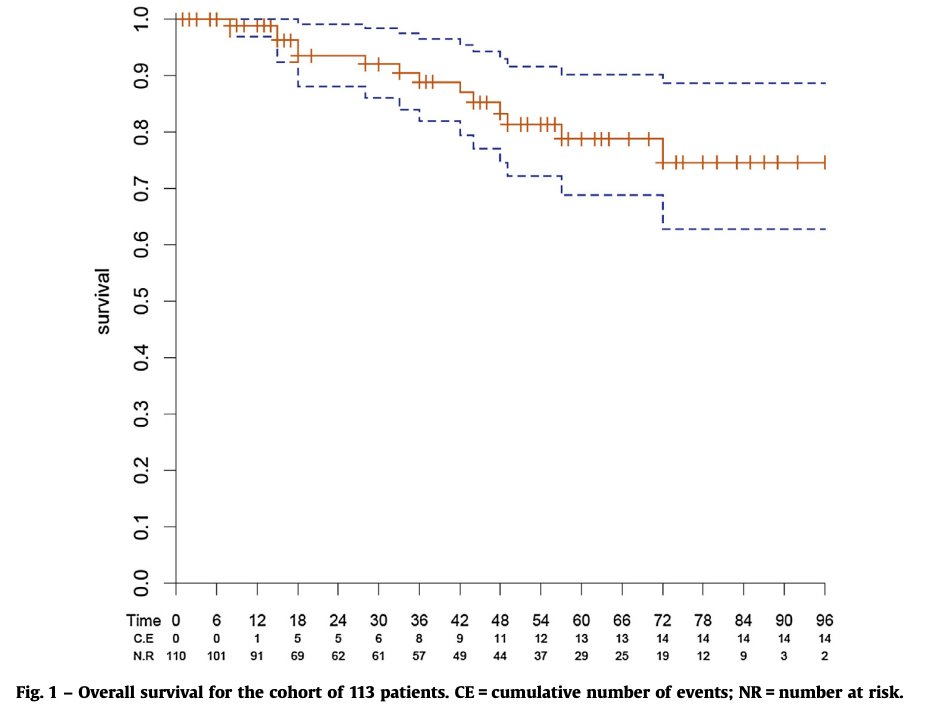
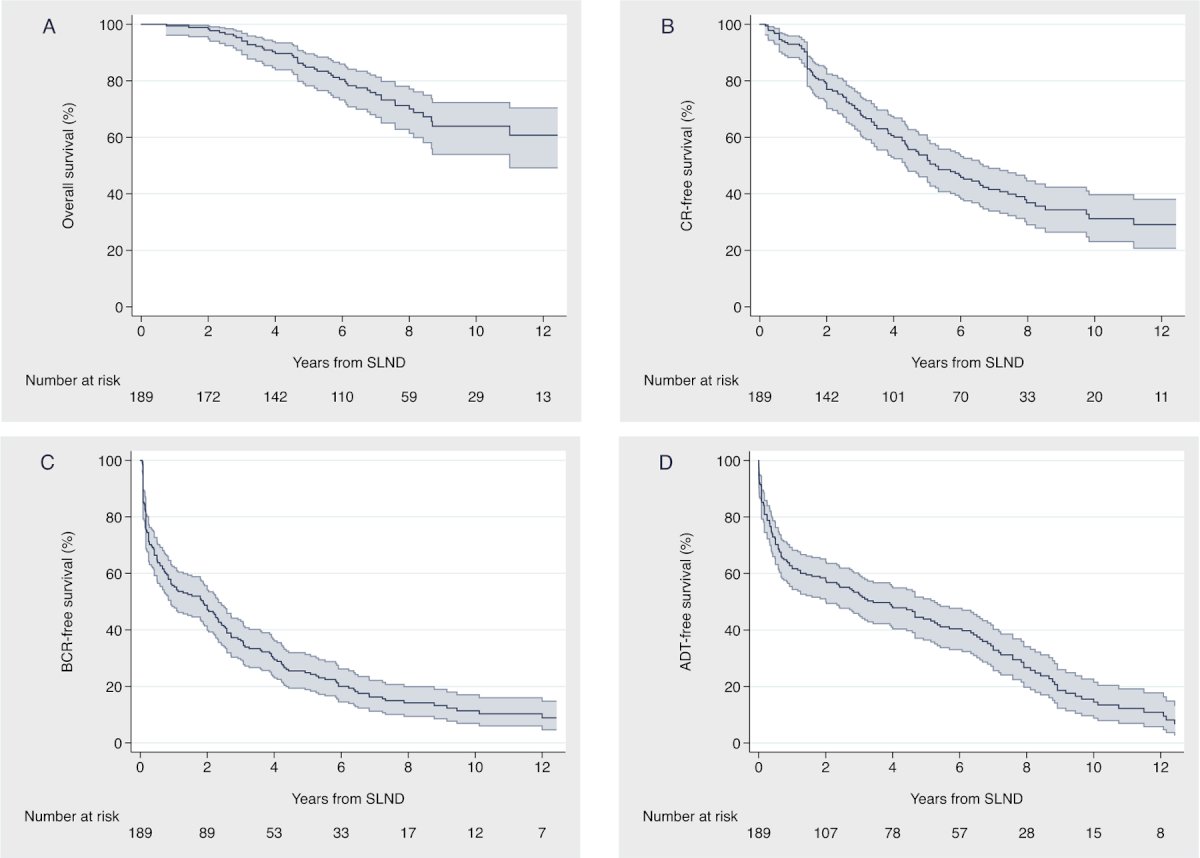
What about salvage lymph node dissection in patients oligorecurrent/metachronous disease? In 2016, Zlattoni et al. published the results of a case series of 117 patients with biochemical recurrence post-RP with cN+ disease detected on 11C-choline PET/CT. All patients underwent a bilateral extended salvage pelvic LN dissection, including 15 patients who had an RPLND. The 5-year BCR-free and CSS rates were 31% and 97%, respectively. Patients with pT2 and GS7 disease had the best outcomes, which may reflect underlying disease biology as opposed to surgical intervention. Another series by Bravi et al. of 189 patients with a median follow-up of 87 months demonstrated that clinical recurrence-free and BCR-free survival rates at 10 years were 31% and 11%, respectively.11
What about metastasis-directed therapy (MDT) in the form of stereotactic body radiotherapy (SBRT) in this setting? There is emerging data from ORIOLE, STOMP, and SABRC-COMET regarding the role MDT in select patients with metachronous, oligometastatic mHSPC.
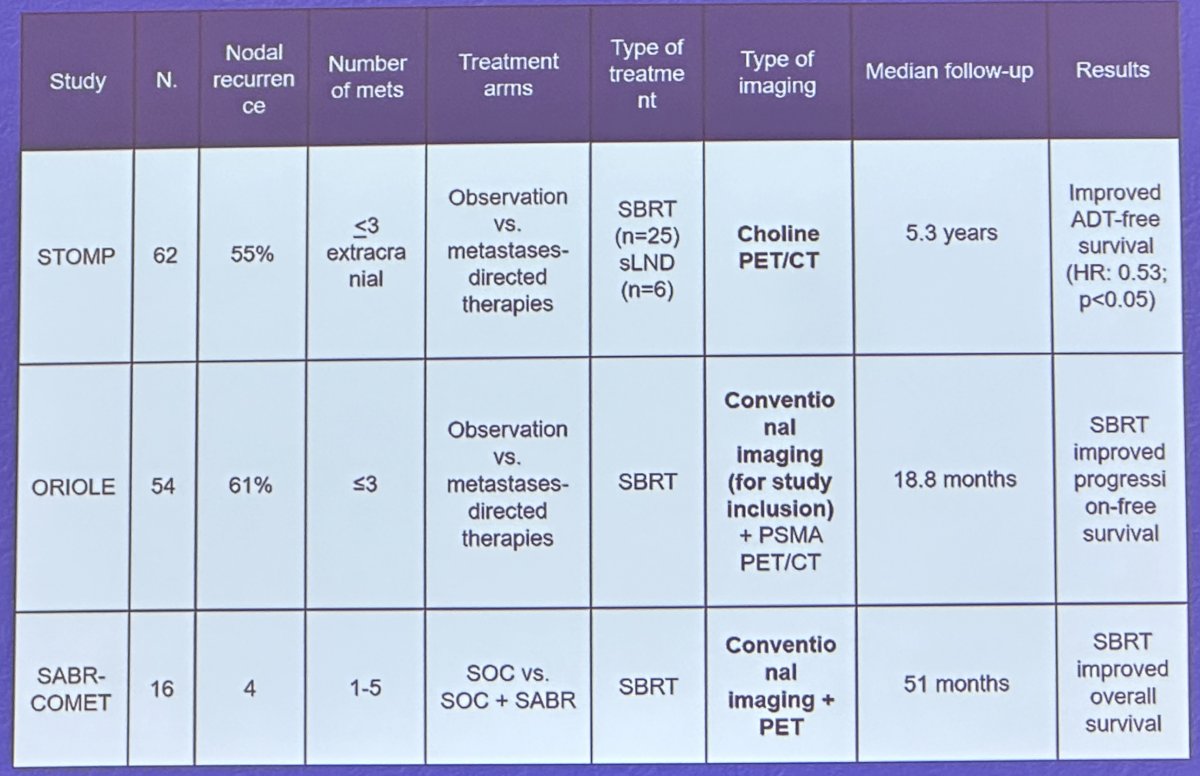
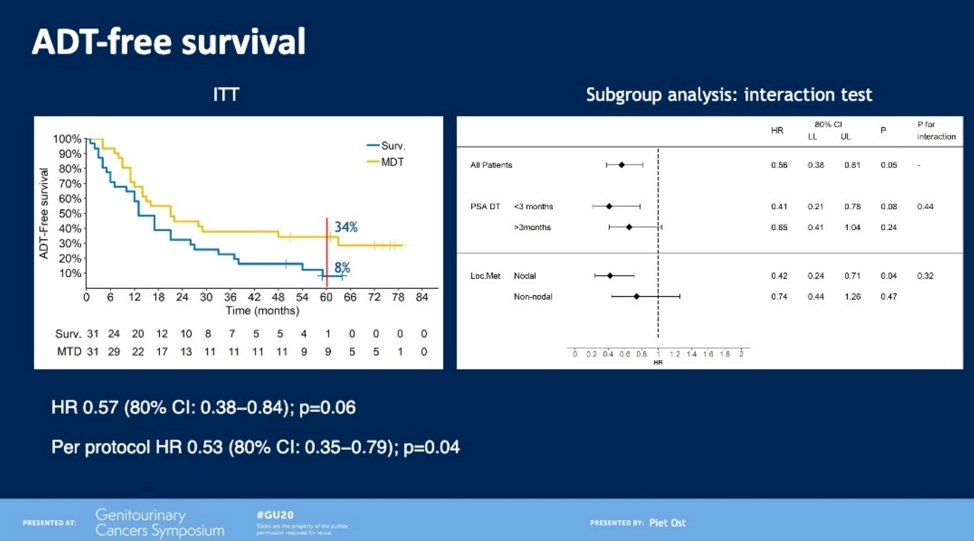
The STOMP trial was a multicenter, randomized phase II trial that prospectively evaluated the effects of MDT for patients with evidence of oligometastatic disease on choline PET/CT (up to three extracranial sites) who had received prior treatment with curative intent and had evidence of biochemical recurrence with testosterone >50 ng/ml (i.e. metachronous, oligometastatic mHSPC). Between 2012 and 2015, 62 patients were randomized 1:1 and MDT was either SBRT or metastasectomy. The primary endpoint was time to initiation of ADT (called ADT-free survival). ADT was initiated for symptoms, progression beyond three metastases, or local progression of known metastatic disease. The updated five-year results were presented at GU ASCO 2020. With a median follow up of 5.3 years, the five-year ADT-free survival was 8% in the surveillance arm compared to 34% for the MDT group (HR 0.57, 95% CI 0.38 to 0.84, log-rank p=0.06). Secondary endpoint of CRPC-free survival at 5 years was 53% in subjects under surveillance and 76% in those receiving MDT (HR 0.62, 80% CI 0.35 to 1.09).12
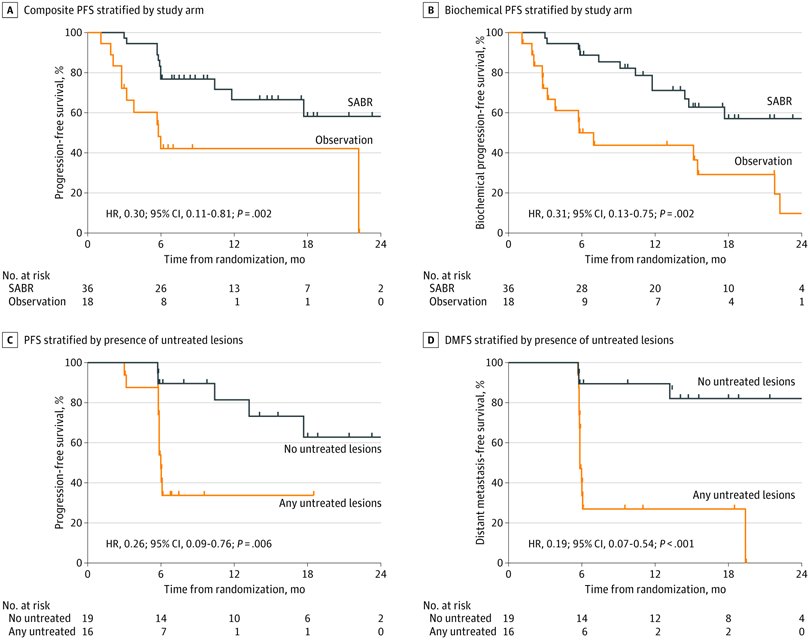
The ORIOLE trial was a randomized phase II trial of 54 men with metachronous, oligometastatic mHSPC (up to three sites). Metastatic sites were diagnosed via conventional imaging. Between 2016 and 2018, patients were randomized in a 2:1 fashion to receive SABR or observation. The primary outcome was progression at 6 months, defined as serum PSA increase, progression detected by conventional imaging, symptomatic progression, ADT initiation for any reason, or death. Progression at six months occurred in 7 of 36 patients (19%) receiving SABR and 11 of 18 patients (61%) undergoing observation (p = 0.005). Treatment with SABR improved median PFS (not reached vs 5.8 months; HR 0.30, 95% CI 0.11 to 0.81).13
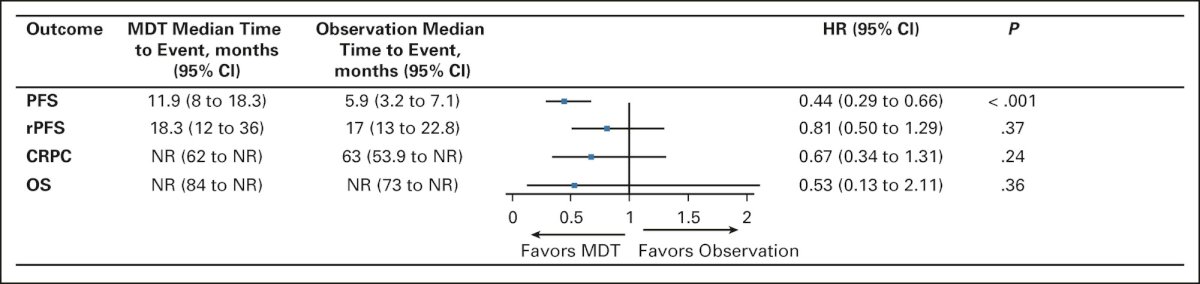
Pooled data from the two trials demonstrate that MDT in these patients improves progression-free survival from 5.9 months (95% CI: 3.2 – 7.1) to 11.9 months (95% CI: 8.0 – 18.3; HR: 0.44, p<0.001), without any significant improvements seen in radiographic progression-free survival, time to castration-resistant disease or overall survival.14
SABR-COMET was a randomized, open-label phase II study of patients with oligometastatic disease (up to five sites) between February 2012 and August 2016. This trial was not restricted to patients with prostate cancer and also included lung, breast, and colorectal cancer patients. Of the 99 patients in this trial, 18 (18%) had prostate cancer. After stratifying by the number of metastases (1–3 vs 4–5), patients were randomized in a 1:2 fashion to receive either palliative standard of care alone or standard of care plus SABR. In an updated analysis published in 2020 (median follow up 51 months), the five-year OS rate was 17.7% (95% CI 6-34%) in the control arm and 42.3% in the SABR arm (95% CI 28-56%, stratified log-rank p=0.006). The corresponding median OS was 28 months and 50 months, respectively.15
Dr. Karnes concluded his presentation with the following take home messages:
- There is a strong biologic rationale for treatment of patients with oligometastatic disease
- There is a high incidence of local symptoms in patients with synchronous/de novo presentations
- Trials of definitive therapy in this disease space are ongoing (SWOG 1802 and TRoMbone)
- If patients are symptomatic Consider RP if feasible
- In patients with metachronous/oligorecurrent disease
- Stronger evidence for radiotherapy in this setting
- May consider surgery for patients with pelvic-only disease
Presented by: R. Jeffrey Karnes, MD, Professor, Department of Urology, Mayo Clinic, Rochester, MN
Written by: Rashid K. Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023
References:- Soloway et al. Stratification of Patients with Metastatic Prostate Cancer Based on Extent of Disease on Initial Bone Scan. Cancer, 1988.
- Boeve LMS et al. Effect on Survival of Androgen Deprivation Therapy Alone Compared to Androgen Deprivation Therapy Combined with Concurrent Radiation Therapy to the Prostate in Patients with Primary Bone Metastatic Prostate Cancer in a Prospective Randomised Clinical Trial: Data from the HORRAD Trial. Eur Urol, 2019.
- Parker CC et al. Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): a randomised controlled phase 3 trial. The Lancet, 2018.
- Mason MD et al. Final Report of the Intergroup Randomized Study of Combined Androgen-Deprivation Therapy Plus Radiotherapy Versus Androgen-Deprivation Therapy Alone in Locally Advanced Prostate Cancer. J Clin Oncol, 2015.
- Ghavamian R et al. Radical Retropubic Prostatectomy plus Orchiectomy Versus Orchiectomy Alone for pTxN+ Prostate Cancer: A Matched Comparison. J Urol, 1999.
- Engel et al. Survival Benefit of Radical Prostatectomy in Lymph Node-Positive Patients with Prostate Cancer. Eur Urol, 2010.
- Schroder FH et al. Screening and Prostate-Cancer Mortality in a Randomized European Study. Eur Urol, 2009.
- Messing EM et al. Immediate Versus Deferred Androgen Deprivation Treatment in Patients with Node-Positive Prostate Cancer After Radical Prostatectomy and Pelvic Lymphadenectomy. Lancet Oncol, 2006.
- Moschini M et al. Prostate Cancer Prostatic Dis, 2017.
- Heidenteich A et al. Cytoreductive Radical Prostatectomy in Men with Prostate Cancer and Skeletal Metastases. Eur Uol Oncol, 2018.
- Bravi CA et al. Long-term Outcomes of Salvage Lymph Node Dissection for Nodal Recurrence of Prostate Cancer After Radical Prostatectomy: Not as Good as Previously Thought. Eur Urol, 2020.
- Ost P, et al. Surveillance or Metastasis-Directed Therapy for Oligometastatic Prostate Cancer Recurrence: A Prospective, Randomized, Multicenter Phase II Trial. J Clin Oncol, 2018.
- Philips R, et al. Outcomes of Observation vs Stereotactic Ablative Radiation for Oligometastatic Prostate Cancer: The ORIOLE Phase 2 Randomized Clinical Trial. JAMA Oncol, 2020.
- Deek MP, et al. Long-Term Outcomes and Genetic Predictors of Response to Metastasis-Directed Therapy Versus Observation in Oligometastatic Prostate Cancer: Analysis of STOMP and ORIOLE Trials. J Clin Oncol, 2022.
- Palma DA, et al. Stereotactic Ablative Radiotherapy Versus Standard of Care Palliative Treatment in Patients with Oligometastatic Cancers (SABR-COMET): A Randomised, Phase 2, Open-Label Trial. Lancet, 2019.


