( UroToday.com) The 2023 American Urological Association (AUA) annual meeting held in Chicago, IL between April 28 and May 1st, 2023, was host to the Arab Association of Urology sectional session. Dr. Karim A. Touijer discussed the current role of lymphadenectomy in the era of PSMA-PET/CT imaging.
Dr. Touijer began by highlighting that the probability of diagnosing pN+ disease is strongly associated with the number of lymph nodes sampled/examined, as demonstrated in the MSKCC cohort.1

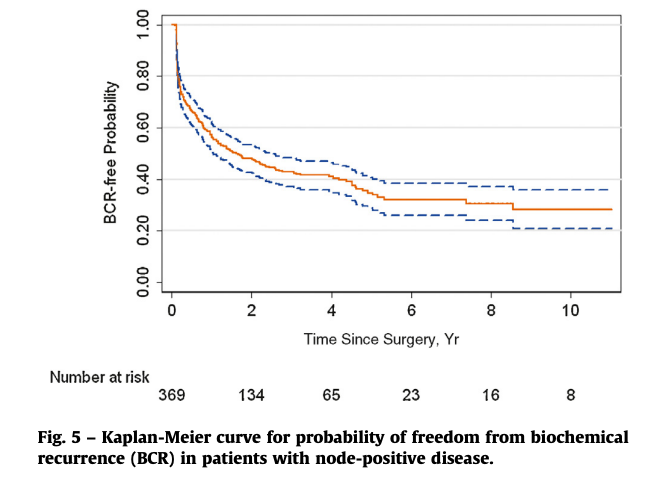
How do patients with pN+ disease treated with radical prostatectomy without adjuvant androgen deprivation therapy (ADT) fare? Long-term analysis from the MSKCC cohort published by Touijer et al. demonstrates that at 10 years, approximately 30% of patients remain without evidence of biochemical recurrence.2 As such, Dr. Touijer suggested that a pelvic lymph node dissection in such patients may be curative in up to 30% of cases.
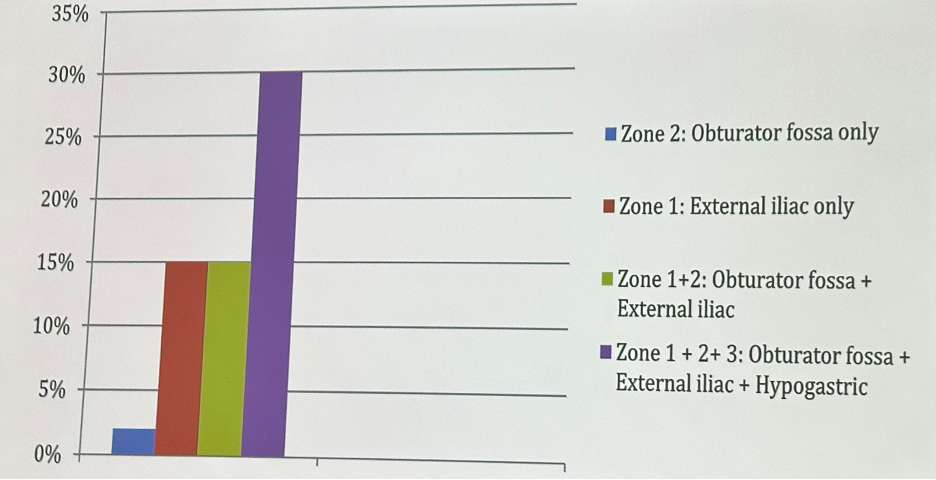
How often is a pelvic lymph node performed at the time of a radical prostatectomy? In a survey of 183 SUO members in 2013, 45% performed PLND on all patients undergoing radical prostatectomy. As to extent of PLND, 15% perform a PLND limited to the external iliac, while 30% include the external iliac, obturator fossa, and hypogastric lymph nodes.3
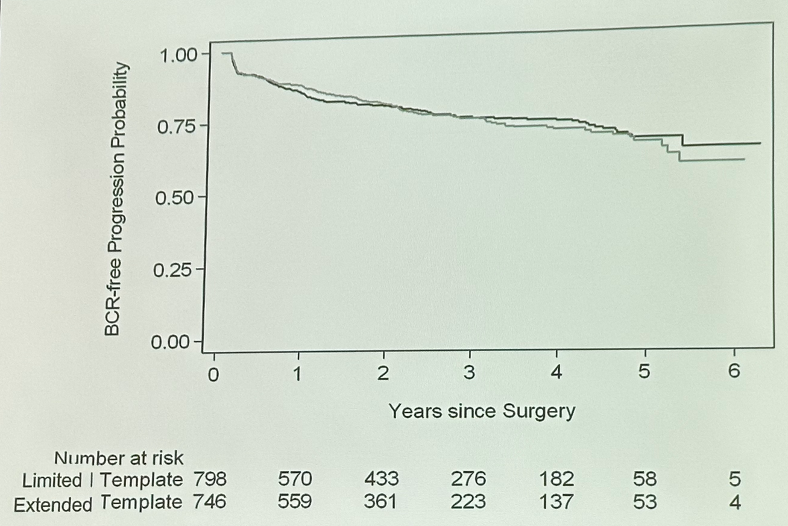
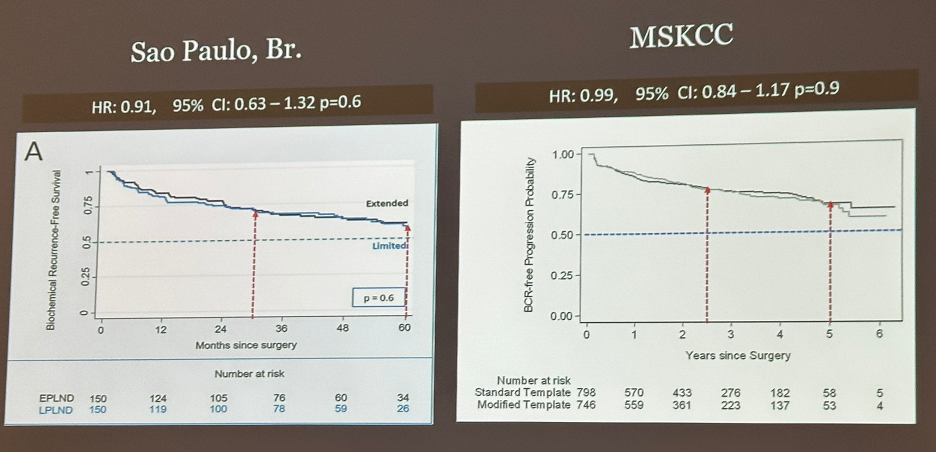
In 2021, Touijer et al. published the results of a randomized controlled trial evaluating limited versus extended PLND. The target accrual was 1,400 patients over five years, with planned one year follow-up after the final accrual. Ultimately, 1,480 patients were accrued between October 2011 and March 2017 (757 in the extended PLND arm and 723 in the limited PLND arm). Patients underwent any of open, laparoscopic, or robotic approaches. The primary endpoint was time to biochemical recurrence (BCR).

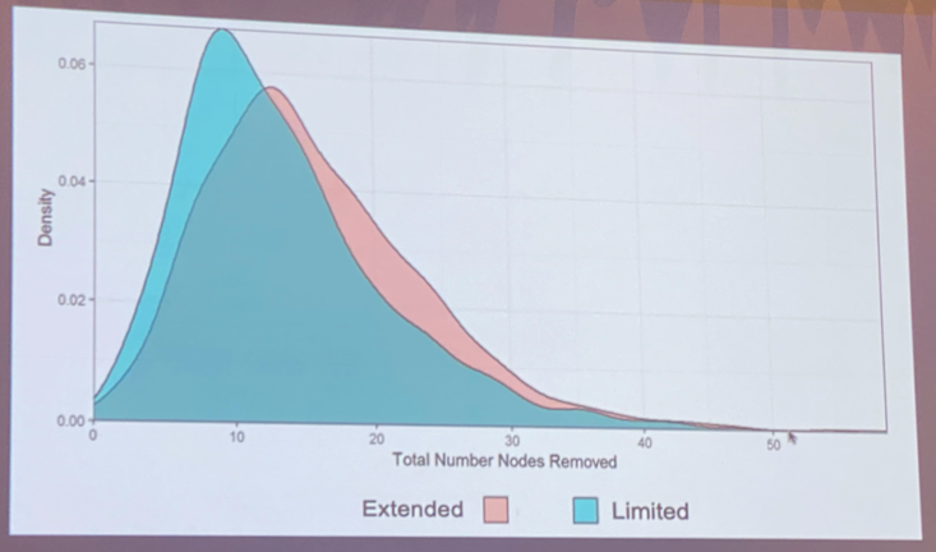
Pathologic nodal disease was present in 103 (14%) extended PLND patients and 81 (11%) of limited PLND patients. This was a negative trial with no significant difference in time to biochemical recurrence between the two arms (HR: 0.99, 95% CI: 0.84 – 1.17, p=0.9). Subgroup analyses failed to identify a subcohort that would benefit from this procedure.4
Dr. Touijer went on to present data from a Brazilian study by Lestingi et al that evaluated this same question in 300 patients (150 in each arm). As opposed to the Memorial study that compared extended PLND to limited PLND, this trial compared superextended PLND to limited PLND.
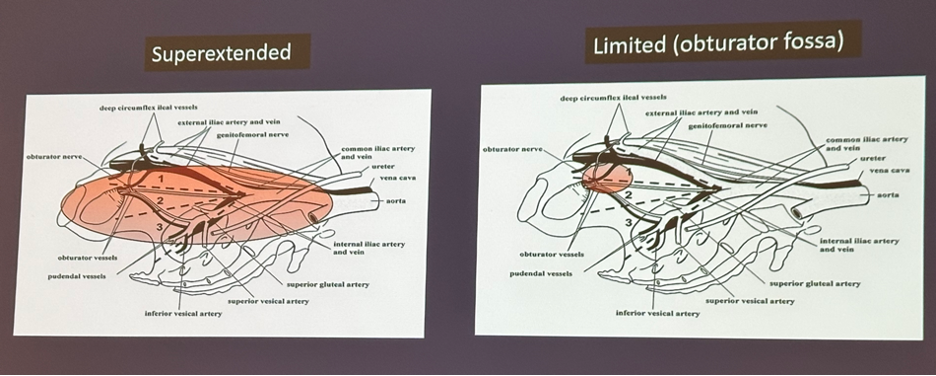
Whereas the positive LN yield was 14% versus 11% in the Memorial cohort, the corresponding rates in the Brazilian trial were 17% and 3.4%, respectively, with the median LN yield 17 in the superextended arm and 3 in the limited PLND arm. Despite this difference, this trial was also negative for the primary outcome with no significant differences in biochemical recurrence-free rates (HR: 0.91, 95% CI: 0.63 – 1.32, p=0.6).
Surgical trials of pelvic lymphadenectomy are difficult to design/conduct and commonly suffer from underpowering, lack of blinding, and surgical imprecision. Given that the two aforementioned trials of a more extensive versus limited PLND failed to show any differences, Dr. Touijer argued that the negative results were likely due to the study designs- specifically the choice of comparator arm. As such, Dr. Toijer and colleagues at MSKCC have since opened a trial of PLND versus no PLND (NCT01407263). Since July 2020, over 600 patients have been enrolled and the trial is on trach to complete accrual within the 5-year window target.
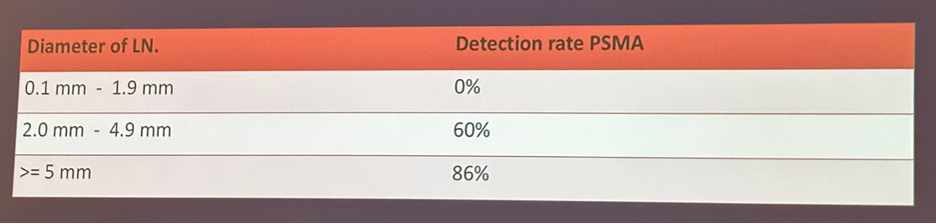
Given the emergence of PSMA-PET/CT, with improved performance characteristics compared to conventional imaging, can we just rely on its findings to guide the decision for PLND? As of yet, it appears that the answer is no, with a 2020 systematic review and meta-analysis of 11 studies demonstrating that 68Ga-PSMA has a wide reported sensitivity ranging between 33% and 100% at the patient-level and between 24% and 96% by LN field.6 This is further complicated by PSMA PET/CT’s poor ability to detect micrometastatic deposits <5 mm in size.
With the advent of PSMA-PET/CT, we have been able to detect tracer-avid noes outside the classic ePLND templates in up to half of cases. These may include mesorectal lymph node metastases that have been previously poorly reported/detected on conventional imaging.
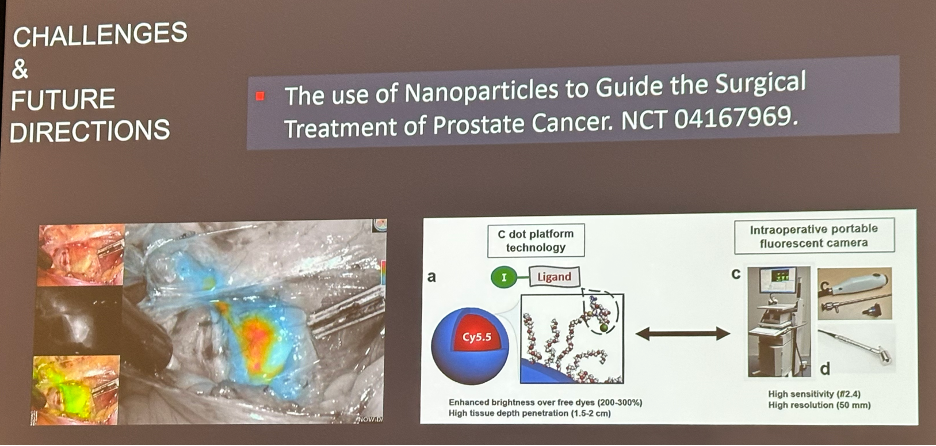
Leveraging the advantages of molecular targeted imaging for improved surgical precision is in the near future with an MSKCC trial currently evaluating the use of nanoparticles to guide the surgical treatment of prostate cancer (NCT04167969).
Dr. Touijer concluded his presentation with the following take home messages:
- PSMA-PET/CT improves the staging capacity of PLND, but, at the current time, may not replace PLND
- Is there a treatment benefit to performing a PLND? As of yet, this remains an unanswered question and a trial of PLND versus no PLND appears to be the better trial design
Presented by: Karim Touijer, MD, MPH, Associate Professor, Memorial Sloan Kettering Cancer Center, New York, NY
Written by: Rashid K. Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023
References:- Masterson et al. The Association Between Total and Positive Lymph Node Counts, and Disease Progression in Clinically Localized Prostate Cancer. J Urol, 2006.
- Touijer et al. Long-Term Outcomes of Patients with Lymph Node Metastasis Treated with Radical Prostatectomy Without Adjuvant Androgen-Deprivation Therapy. Eur Urol, 2014.
- Touijer et al. Urol, 2013.
- Touijer et al. Limited versus Extended Pelvic Lymph Node Dissection for Prostate Cancer: A Randomized Clinical Trial. Eur Urol Oncol, 2021.
- Lestingi JFP et al. Extended Versus Limited Pelvic Lymph Node Dissection During Radical Prostatectomy for Intermediate- and High-risk Prostate Cancer: Early Oncological Outcomes from a Randomized Phase 3 Trial. Eur Urol, 2021.
- Luiting et al. Use of Gallium-68 Prostate-Specific Membrane Antigen Positron-Emission Tomography for Detecting Lymph Node Metastases in Primary and Recurrent Prostate Cancer and Location of Recurrence After Radical Prostatectomy: An Overview of the Current Literature. BJU Int, 2020.


