(UroToday.com) Dr. Arun Chawla began the session with an interesting presentation on the use of ureteral stents. Chawla stated that in the world of urology, endourologists routinely use stents. Although urologists justify doing so because it promotes the passage of stone fragments, lowers stricture formation, prevents obstructions, and reduces renal colic, Chawla believes it to be a hypothetical fact. Chawla conducted a single center prospective randomized control study to compare patients with or without a stent after undergoing uncomplicated retrograde semi rigid ureteroscopy (URS). Specifically, the study investigated cases with patients who had distal ureteric calculus of sizes less than 1 cm. Furthermore, the study considered complication rates, additional interventions, pain (using the visual analog scale, VAS), sexual function, and emergency visits between the two groups.
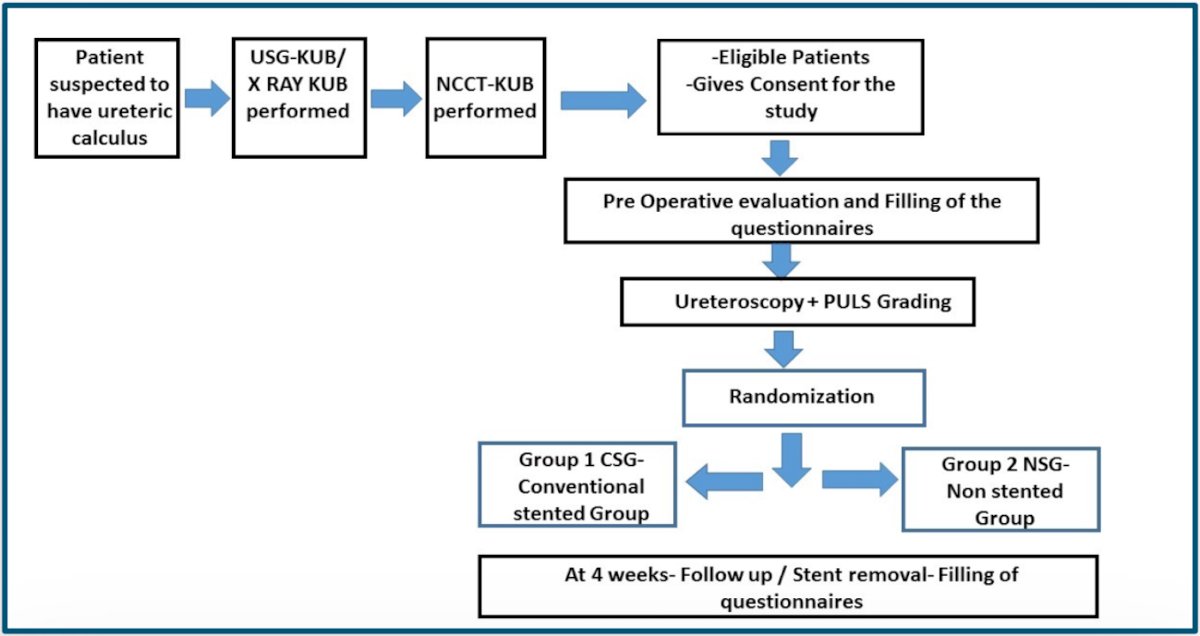
The recruitment of patients was quite tedious (refer to image below). Once suspicions of a ureteric calculus within a patient was confirmed via imaging, patients who consented for the study were asked to fill out questionnaires. Patients underwent ureteroscopy and a PULS grade was given once the procedure was complete, and it was at that moment Chawla randomized patients into the conventional stent group (CSG) and the non-stented group (NSG). After 4 weeks, a scheduled follow-up was performed for patients to, if applicable, remove stents and fill out questionnaires such as the: The Male Sexual Health Questionnaire - ejaculatory dysfunction (MSHQ-EjD), Female Sexual Function Index (FSFI) International Prostate Symptom Score (IPSS), the International Index of Erectile Function (IIEF-5) and
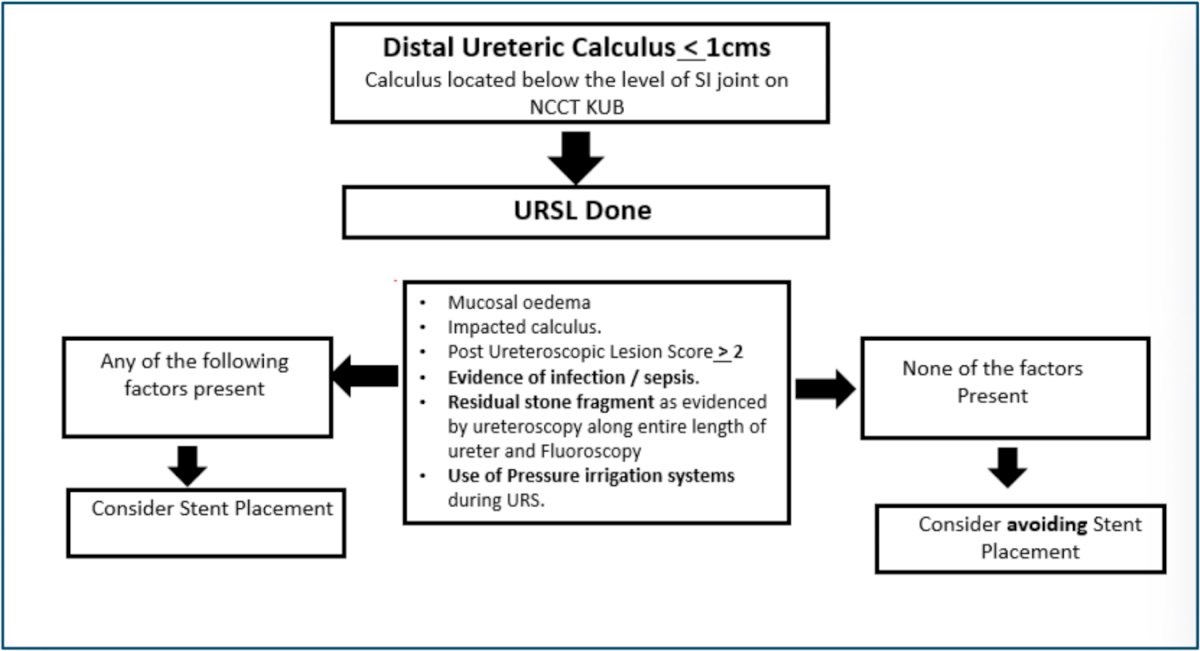
The image below demonstrates the logical flow of patient placement. It is important to note that patients who experienced ≥ 2 PULS, residual stone fragments, sepsis, had the use of pressure irrigation during the procedure, and other factors listed in the middle square were considered for placement into the stent placement group.
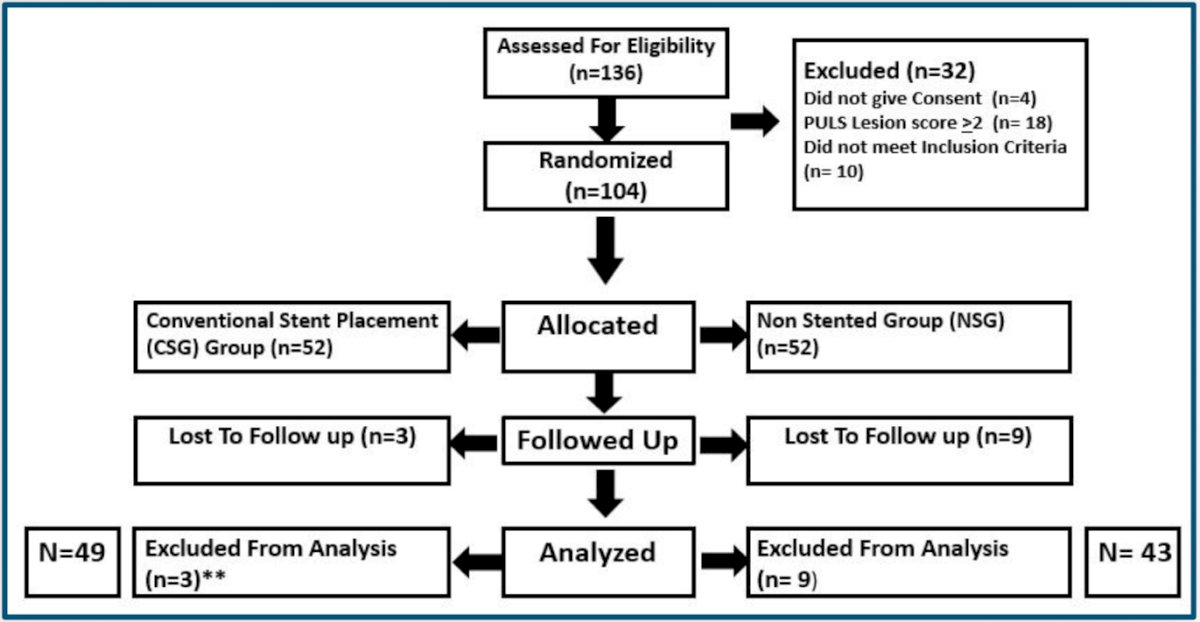
A total of 136 patients were assessed for eligibility however only 104 were selected and randomized for the study with 52 patients in each group. After group placement and follow-up, 49 patients remained in the conventional stent placement group and 43 patients remained in the non-stented group (total of 92 patients). The questionnaires' results were assessed using generalized estimating equations to investigate the difference between the two groups.
The IPSS showed a difference within frequency, urgency, nocturia, and storage symptoms with the total IPSS Score (p<0.001) and quality of life score (p=0.002) being significant; these results demonstrated the scores were worse for the CSG. Of the MSHQ-EjD, there was a significant difference in ejaculation bother/ satisfaction (p=<0.001) and of the FSFI, lubrication, and satisfaction were significant, (p<0.001 and p=0.006 respectively) with an overall score of significance (p=0.004). The results had no significant difference among visits to the emergency room, secondary interventions, VAS, analgesia, and readmissions. Refer to the table below for a comprehensive analysis of the findings.

With these results, Chawla recommends that stent use could be avoided following uncomplicated URS, defined as: no stone impaction, no remaining fragments, no injections, complete ratio and fluoroscopic absence of stone, and no injury (PULS 2 ≥).
Following the presentation, Dr. Bernardo (serving as a moderator) asked if alpha blockers were prescribed to compare the results of symptoms. Dr. Chawla responded that none of the patients were given alpha blockers, instead, they received tramadol. Dr. Bhojani (serving as a moderator) further inquired about the randomization of the patients, asking how many patients had to be considered before the final groups were selected. Dr. Chawla emphasized that patients were randomized only after URS was completed and patients that experienced signs of impaction, infection, inflammation, and injury were excluded from the study (making up nearly 40% of patients).
Presented by: Arun Chawla, MD, Kasturba Medical College of Manipal
Written by: Seyed Amiryaghoub M. Lavasani, B.A., University of California, Irvine, @amirlavasani_ on Twitter during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023


