(UroToday.com) The 2024 American Urological Association (AUA) Annual Meeting held in San Antonio, TX between May 3rd and 6th, 2024 was host to a non-invasive bladder cancer moderated poster session. Julia Nadelmann presented a study of the financial toxicity of non-muscle invasive bladder cancer (NMIBC) in a diverse urban population.
It is currently estimated that there are over 70,000 incident cases of bladder cancer annually, with 75% of such cases falling under the NMIBC category. The recurrence rate for treated NMIBC is estimated to be between 70 and 80%, and, as such, the management of NMIBC mandates repeat endoscopic procedures for surveillance. On a per-patient basis, bladder cancer is estimated to have one of the highest associated lifetime costs amongst all malignancies, in part due to the need for long-term surveillance. It is estimated that a single NMIBC patient’s lifetime cost is $120,000.
Financial toxicity assesses the negative impact of treatment costs on patients’ lives and has been used across several diseases and cancer types. Patients endorsing financial toxicity are more likely to experience delays in care, medication rationing, and lower quality of life. The most comprehensive study to previously evaluate financial toxicity among all bladder cancer patients found that 24% of bladder cancer patients endorsed financial toxicity. However, this study evaluated patients with both muscle-invasive and NMIBC. Additionally, 89% of patients were Caucasian.1 The goal of this study was to characterize the financial toxicity of NMIBC in a diverse urban population.
The investigators surveyed a cohort of patients from Montefiore Medical Center between July 2022 and April 2024 using the validated COST tool, which assesses both direct and indirect costs of treatment. Direct costs are those that refer to actual out-of-pocket costs of treatment, whereas indirect costs include treatment-associated costs, such as the cost of transport to the office for procedures or lost income from missed days of work. In addition to the COST tool, patients’ demographic information, disease-specific information, and estimated out-of-pocket costs were collected. Descriptive statistics, X2 tests, T T-tests, Spearman correlation, and logistic regression were performed using SPSS.
Sixty-four patients with NMIBC were surveyed. The median age was 74 years (IQR: 64–80). 45% of patients were female, with 42% identifying as Caucasian, 30% as Black, and 28% as Hispanic.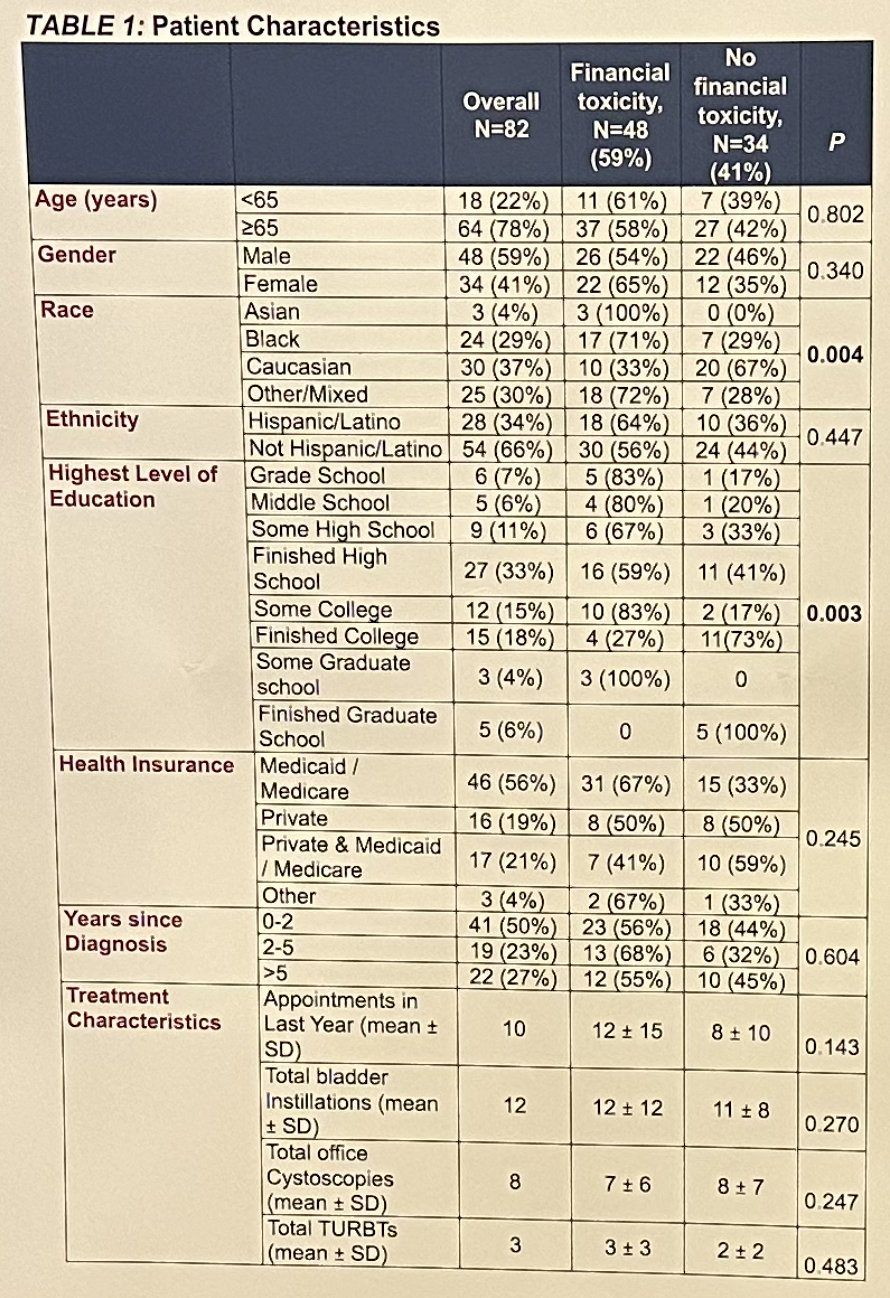
The median COST score was 23.2 (IQR: 15–32). 59% of patients reported at least moderate financial toxicity (COST score ≤25), and 36% reported severe financial toxicity (COST score <14). Black patients were more likely to experience at least moderate FT, compared to Caucasians (79% vs 33%, p<0.05). Caucasian patients had a mean COST score 9 points higher than all other races aggregated (p<0.01).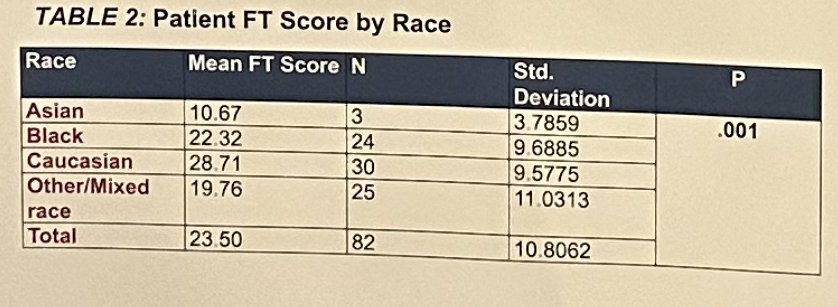
Overall median household income was $38,000 (IQR, $20,000-$72500), and increasing income had a significant positive correlation with the COST score (Pearson’s R=0.469, p<0.001). Risk factors for financial toxicity included non-Caucasian race and lower education level.
The investigators concluded that:
- The rates of financial toxicity in this cohort of bladder cancer patients were higher than those previously reported (59% vs. 24% in previously reported literature)1
- Financial toxicity may disproportionately affect non-Caucasian individuals with lower educational levels, which is consistent with previous research findings
- Financial toxicity does not appear to be related to gender, age, insurance status, or treatment characteristics
- Future work will focus on better elucidating how financial toxicity in NMIBC patients may be related to decreased access to care
- Addressing financial toxicity in NMIBC within this diverse patient population should shape both screening and treatment guidelines
- There is potential for patients with risk factors to be proactively screened in order to be connected with hospital support services, such as fee assistance programs and hospital transport programs
- NMIBC patients with financial toxicity may benefit from the development of accurate, less invasive methods of NMIBC surveillance (e.g., development of at-home urine-based biomarkers rather than cystoscopy)
Presented by: Julia Nadelmann, Medical Student, Albert Einstein College of Medicine, Bronx, NY
Written by: Rashid Sayyid, MD, MSc - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, May 3rd - 6th, 2024
References:
- Casilla-Lennon MM, Choi SK, Deal AM, et al. Financial Toxicity among Patients with Bladder Cancer: Reasons for Delay in Care and Effect on Quality of Life. J Urol. 2018;199(5): 1166-73.


