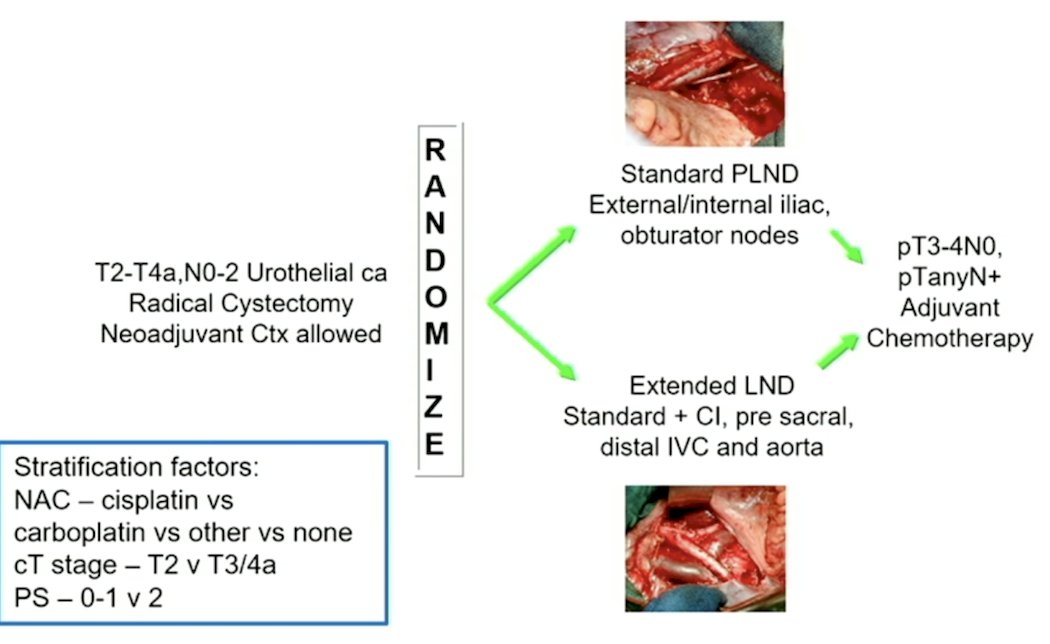
(UroToday.com) The 2024 American Urological Association (AUA) annual meeting featured a session on invasive bladder cancer, and a presentation by Dr. Leilei Xia discussing an exploratory analysis of the SWOG S1011 trial assessing the national performance of lymphadenectomy for muscle-invasive urothelial cancer to define an optimal lymph node yield. The SWOG S1011 trial previously showed that extended lymphadenectomy provided no benefit compared to standard lymph node dissection in patients with muscle-invasive bladder cancer undergoing radical cystectomy based on the primary objective of disease free survival. The study design for SWOG S1011 is as follows:
The median lymph node yield in the SWOG S1011 standard lymph node dissection arm was 24 (range 6-61), which was significantly higher than in previous studies. The high lymph node yield can be attributed to:
- High-quality lymph node dissection
- Expert credentialed surgeons performing radical cystectomy
- Pathology reviews performed by experienced pathologists
Dr. Xia and colleagues hypothesized that the national performance of lymph node yield is unlikely to match the results of the SWOG S1011 trial.
This study identified patients with cT2-4aN0-2 urothelial cancer who underwent open radical cystectomy and lymph node dissection with or without neoadjuvant chemotherapy (the same eligibility as SWOG S1011) from the NCDB from 2010-2019. Patients were only included if they had a lymph node yield of 6 to 61, mirroring the standard lymph node dissection arm of SWOG S1011. Further exploratory analyses were performed to define optimal lymph node yield by adjusting the lower range of lymph node yield to match the median lymph node yield in the SWOG S1011 trial.
There was a total of 6,083 patients from 690 hospitals included in the analysis. Lymph node yield distribution was as follows: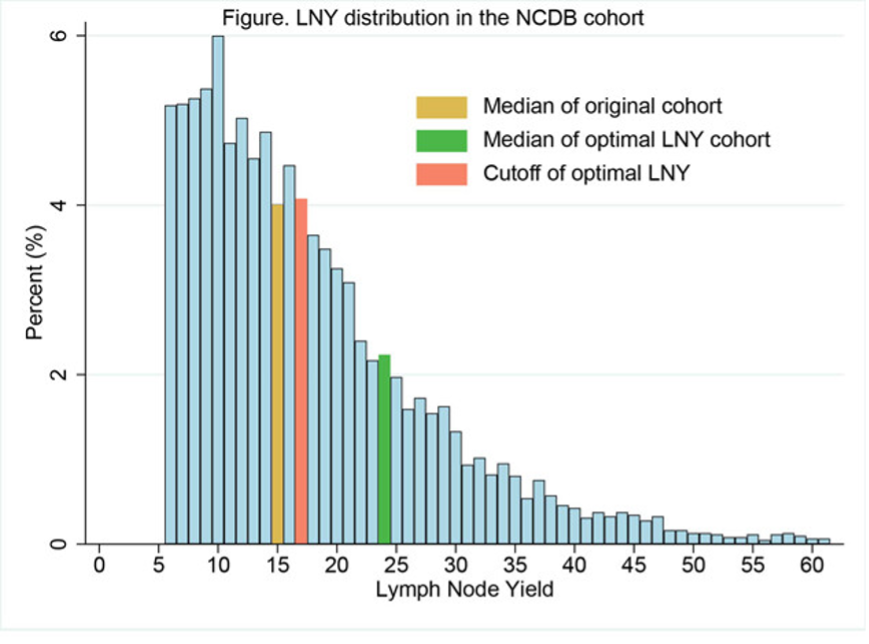
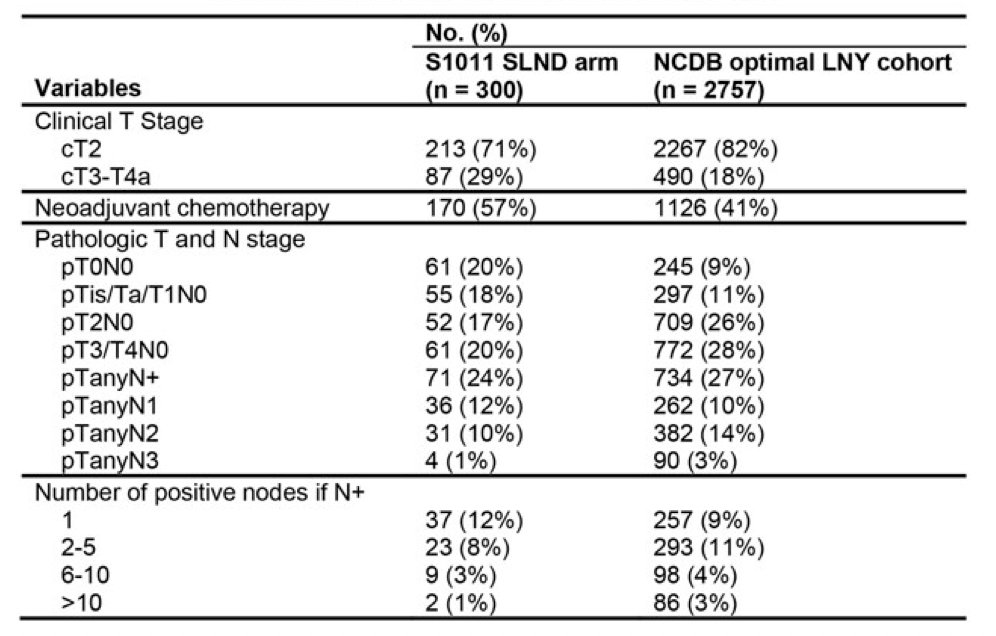
Median lymph node yield was 15, which was 9 nodes less than the SWOG S1011 standard lymph node dissection arm. To match the median lymph node yield of 24 in SWOG S1011, the lower range for NCDB cohort had to be adjusted to 17 nodes, thus defining optimal lymph node yield as lymph node yield ≥ 17. A total of 2,757 patients (45.3%) had optimal lymph node yield, and 404 hospitals (58.6%) had at least one patient with optimal lymph node yield. There were no significant differences in lymph node positive patients between NCDB optimal lymph node yield cohort and the SWOG S1011 standard lymph node dissection arm (27% vs 24%, p = 0.27) suggesting the potential adequacy of using lymph node yield ≥ 17 for staging. The following table shows the comparison of clinical and pathological variables between the NCDB optimal lymph node yield and the SWOG S1011 standard lymph node dissection arm:
Multivariable logistic regression showed higher hospital radical cystectomy volume, more recent years of diagnosis, and neoadjuvant chemotherapy (OR 1.22, p=0.001) were associated with higher odds of achieving optimal lymph node yield.
Dr. Xia concluded this presentation by discussing an exploratory analysis of the SWOG S1011 trial assessing the national performance of lymphadenectomy for muscle-invasive urothelial cancer to define an optimal lymph node yield with the following take-home messages:
- Real-world data indicates that the national performance of lymph node dissection for muscle-invasive bladder cancer in the United States, as evaluated by lymph node yield, does not meet the standards set by the SWOG S1011 trial
- This suggests a significant opportunity for improvement in real-world practice
- Although not perfect, establishing an optimal lymph node yield for lymph node dissection could potentially enhance the quality of lymph node dissection nationally
- Further studies are required to rigorously define what constitutes an optimal lymph node yield
Presented by: Leilei Xia, MD, University of Pennsylvania Health System, Philadelphia, PA
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 – Mon, May 6, 2024.


