(UroToday.com) The 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX between May 3 and May 6, 2024, was host to the Bladder Cancer Non-invasive podium session. Dr. Sanjay Das presented the results of a propensity-scored matched analysis comparing white light cystoscopy (WLC) versus blue light cystoscopy (BLC) recurrence outcomes among non-muscle invasive bladder cancer (NMIBC) patients within an equal access healthcare setting: the Veterans Affairs (VA) healthcare system.
Recent conflicting evidence has emerged regarding the efficacy of BLC and its influence on oncological outcomes. In this study, Dr. Das and colleagues aimed to elucidate the recurrence outcomes in a predominantly high-risk NMIBC patient population who underwent either blue light or white light cystoscopy. Dr Das stated that despite existing guideline recommendations for BLC, real-world data comparing BLC vs WLC is lacking. The investigators conducted the BRAVO (Bladder cancer recurrence analysis in veterans and outcomes) study. The outcomes of interest were recurrence, progression, and overall survival among NIMBC patients in the VA healthcare system.
In this retrospective cohort study, the authors abstracted data from NMIBC patients who underwent either blue light or white light cystoscopy between 1997, and 2021. Initially, 378 patients who had undergone BLC were identified as well as 587 patients who had undergone BLC. After 1:1 propensity score matching 313 patients in the BLC group were matched to 313 in the WLC group. The variables utilized to calculate the propensity score included:
- Age at diagnosis
- Gender
- Race/ethnicity.
- Location of bladder cancer diagnosed (within a VA facility versus outside VA)
- Smoking status
- Clinical grade group
- BCG treatment (yes/no)

Patients were eligible for the study if they had undergone TURBT before December 2021, received BLC according to CPT codes, and had at least 1 year of continuous follow-up within the VA healthcare system. Time to recurrence following either blue light or white light cystoscopy was calculated from the date of bladder cancer diagnosis. Survival analysis using the Kaplan-Meier method was used to estimate event-free survival. They conducted three Cox proportional hazard regressions to evaluate the association between cystoscopy modality (blue versus white light) and recurrence rates. The first regression was non-adjusted, the second one was adjusted for propensity score as weight, receipt of BCG, and/or definitive treatment, and the third one was adjusted for baseline covariates (described above).
Dr. Das reported that the median follow-up was 3.4 years for the BLC and 2 years for the WLC groups. After propensity score matching, the groups appeared well-balanced. Overall, 39% had low-risk disease (TaLG) 71% high-risk disease (CIS, T1, or TaHG), and 52% received BCG during the study. The median patient age at diagnosis was 71 (BLC) and 72 (WLC) years, 99% were male and 11% were black, consistent with the VA patient demographics, 9 (WLC) vs 11% (BLC) of patients had CIS +/- papillary disease, and 54% (WLC) and 53% (BLC) had HG Ta/T1 disease +/- CIS.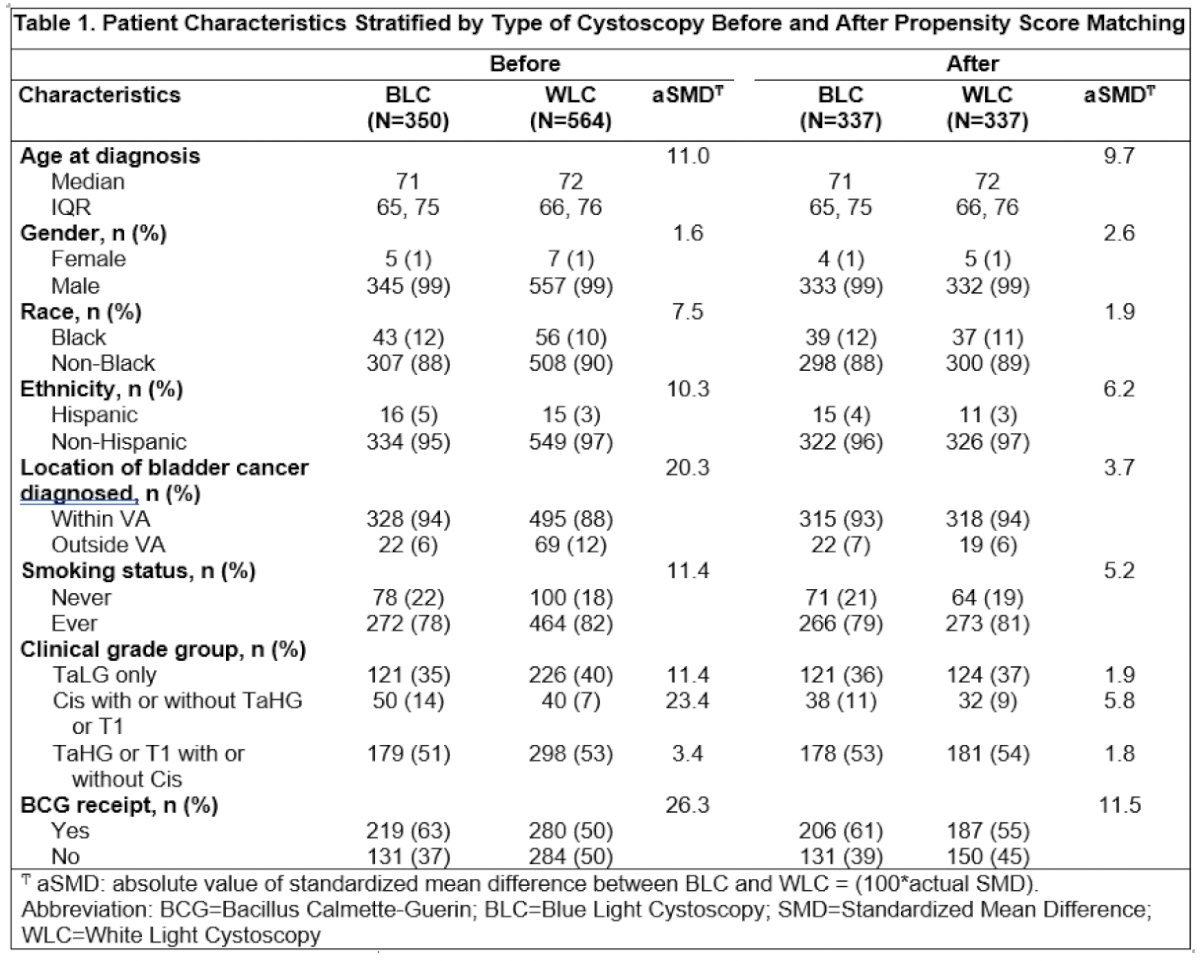
On multivariable analysis, the risk of recurrence was significantly lower following BLC (HR: 0.63; 95% CI: 0.51 to 0.89, p=0.006) compared to WLC.

Dr. Das showed results of PFS and OS, indicating that the risk of progression was significantly lower following BLC (HR: 0.51) compared to WLC on multivariable analysis. The same trend was observed for OS (HR 0.41).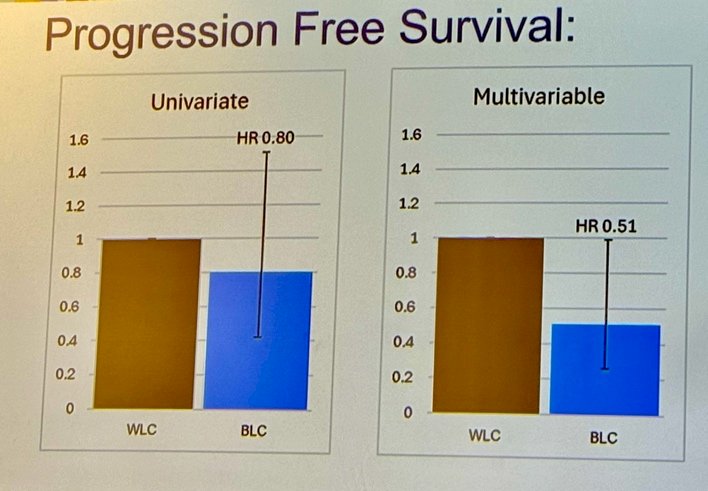
 After adjusting for propensity score as weight, receipt of BCG, and definitive treatment, BLC reduces the risk of recurrence (HR 0.59) and progression (HR 0.56).
After adjusting for propensity score as weight, receipt of BCG, and definitive treatment, BLC reduces the risk of recurrence (HR 0.59) and progression (HR 0.56).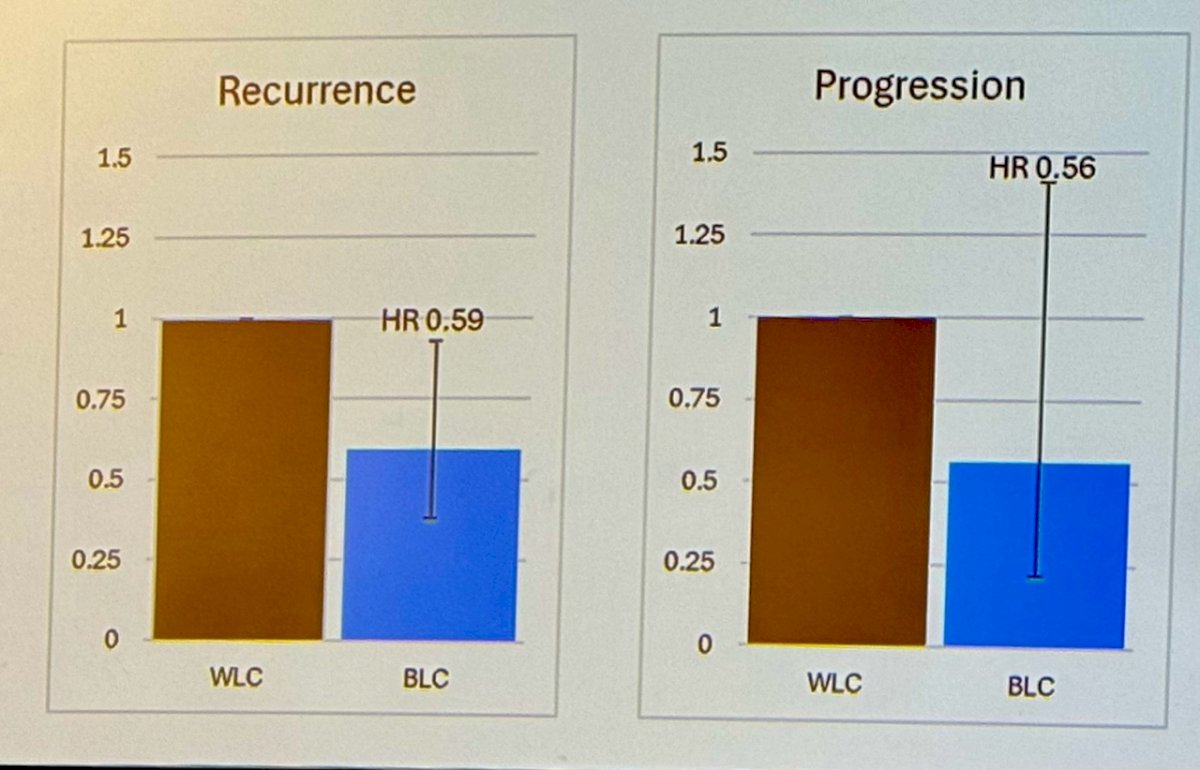
Dr. Das explained that they measured BCG exposure, with 61% having received BCG in the BLC group compared to 43% in the WLC group. Subsequent definitive therapy was used more frequently in the BLC arm (51% vs. 32%), which could potentially lead to better oncological outcomes in the BLC arm.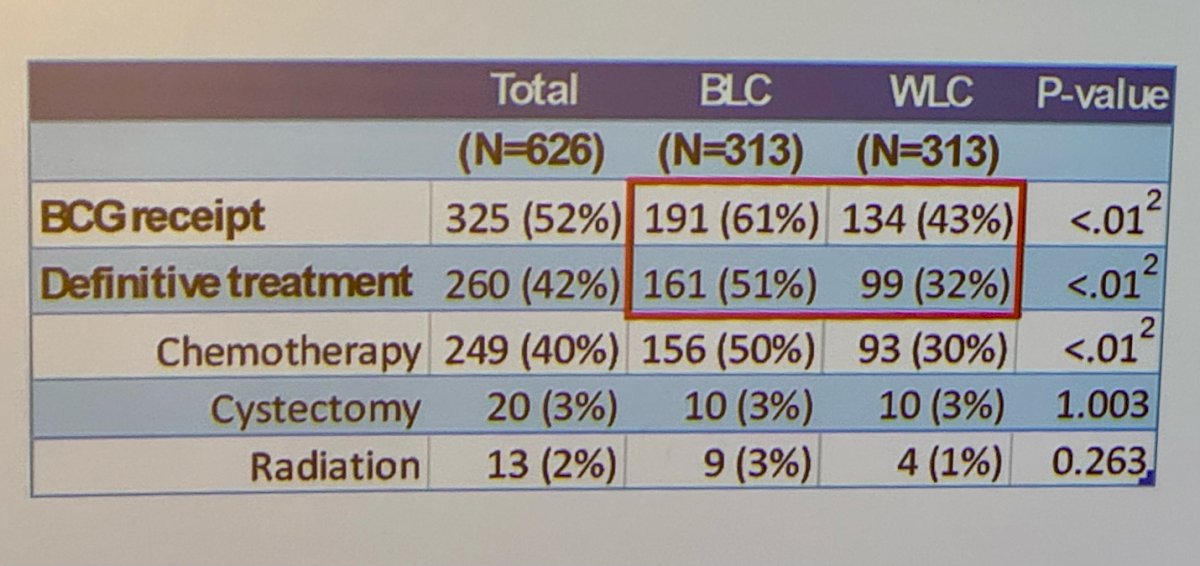
Dr. Das ended his presentation concluding that there is a significantly decreased risk of recurrence progression and improved overall survival in NMIBC patients who underwent blue light versus white light cystoscopy when treated in the context of the equal access VA healthcare setting which is the largest equal access setting in the United States of America.
Presented by: Sanjay Das, MD, Urologic Oncology Fellow, University of California, Los Angeles, Los Angeles, CA
Written by: Julian Chavarriaga, MD - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @chavarriagaj on Twitter during the 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX between May 3rd and May 6th, 2024
Related content: VA BRAVO 2 Study: Blue Light Cystoscopy Improves Outcomes in NMIBC Patients in Equal Access Setting - Stephen Williams


