(UroToday.com) The 2024 American Urological Association (AUA) Annual Meeting held in San Antonio, TX between May 3rd and 6th, 2024 was host to a non-invasive bladder cancer podium session. Dr. Yudai Ishikawa presented the results of an analysis evaluating the diagnostic performance of fluorescence cystoscopy using oral 5-aminolevulinic acid (ALA) in transurethral resection of bladder tumor (TURBT) after BCG treatment.
Fluorescence cystoscopy using oral 5-ALA has been demonstrated in numerous studies to improve the sensitivity for the detection of urothelial carcinoma of the bladder. However, the diagnostic performance of fluorescence cystoscopy using oral 5-ALA for TURBT after BCG treatment requires further evaluation. In this study, Dr. Ishikawa and colleagues evaluated the diagnostic accuracy of fluorescence cystoscopy using oral ALA in TURBT following BCG treatment in comparison to white-light endoscopy.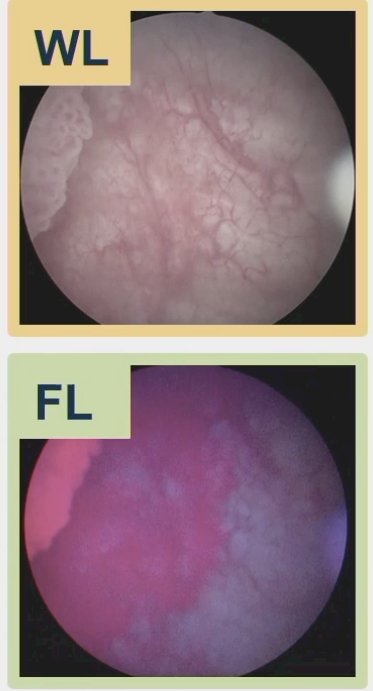
The investigators included 302 patients with NMIBC who underwent fluorescence cystoscopy-guided TURBT with oral 5-ALA at a single academic center between 2018 and 2023. 5-ALA was administered at a dose of 20 mg/kg orally two hours prior to TURBT. A total of 1,469 lesions were sampled from the 302 patients included.
White light and fluorescence cystoscopy findings were recorded separately during the TURBT. Tissue samples were obtained from all lesions with abnormal findings on either white light or fluorescence cystoscopy. Random biopsies were also performed in select patients. The sensitivity, specificity, positive, and negative predictive values for the diagnosis of urothelial carcinoma of the bladder were compared between white light and fluorescence cystoscopy in patients with and without prior BCG treatment. The diagnostic performances of both modalities were further evaluated based on the time from last BCG instillation to TURBT.
The baseline patient characteristics by prior history of BCG treatment are summarized below. The median patient age was 73 years, and 250 patients (83%) were male. Overall, 63 patients had a prior history of BCG treatment; among them, the median time from the last BCG intravesical injection was 24 months and maintenance BCG was administered in 19 patients (30%).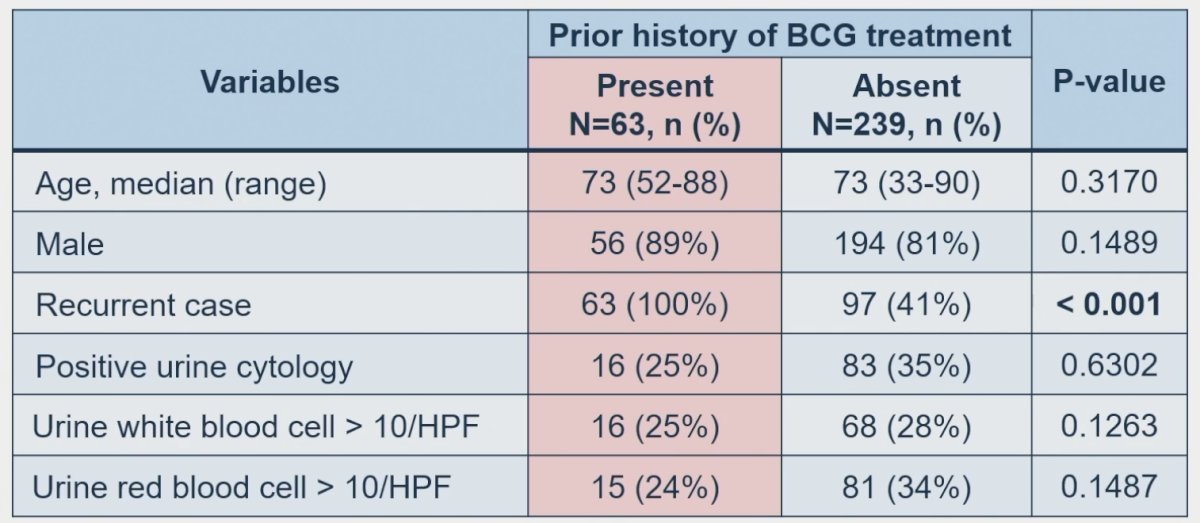
Among 1,469 lesions resected, 478 lesions were diagnosed as cancer (Ta: 73; T1: 264; CIS: 141).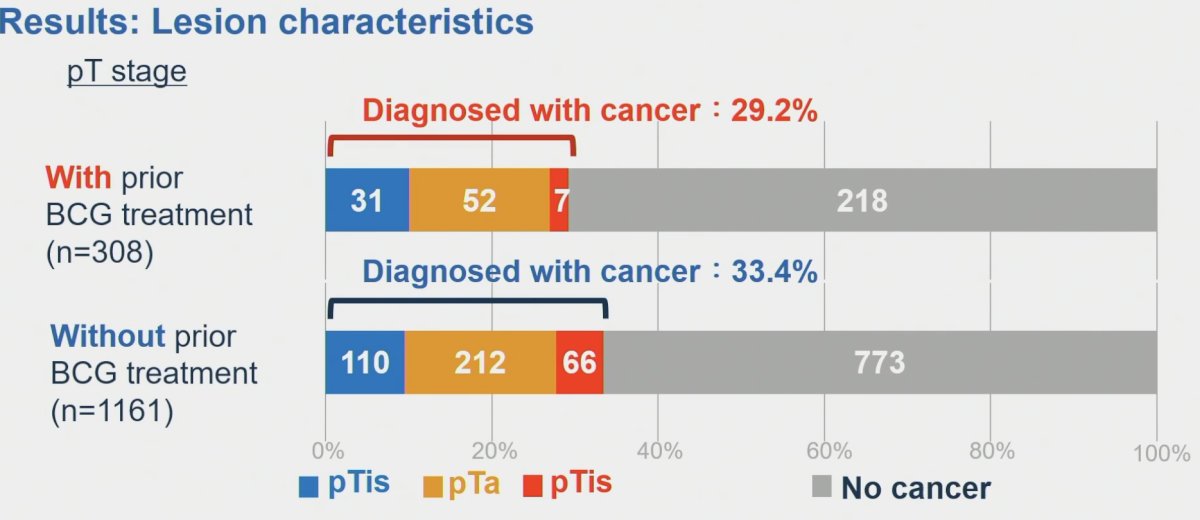
The sensitivity and specificity for white light and fluorescence cystoscopy-guided TURBTs were:
- No prior BCG
- Sensitivity: 78% and 87%
- Specificity: 74% and 70%
- Prior BCG
- Sensitivity: 88% and 87%
- Specificity: 68% and 62%
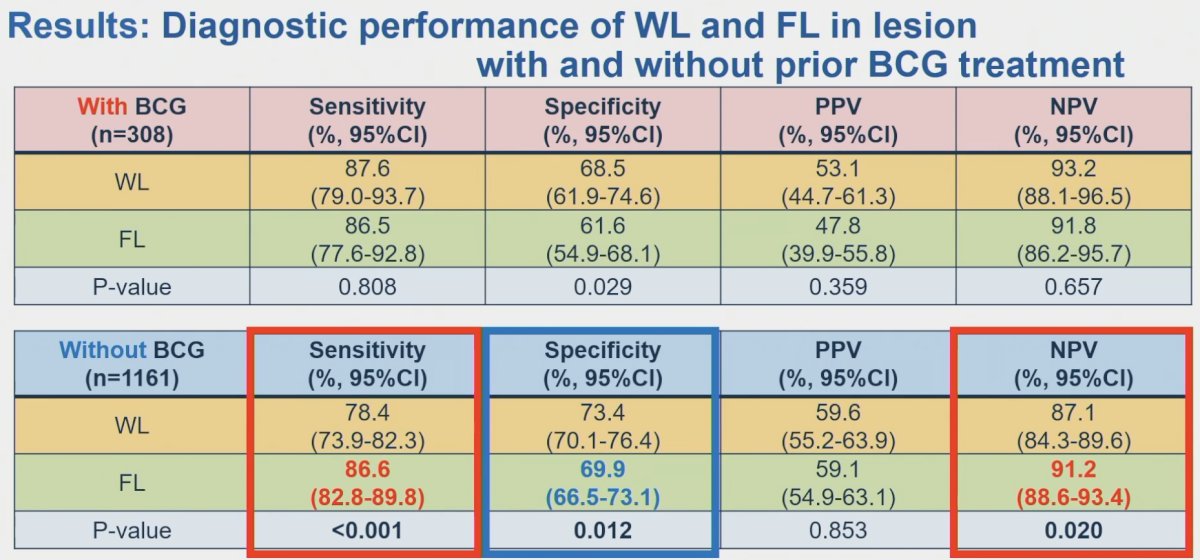
In the patients with prior BCG treatment, there were no specific trends in sensitivity and specificity by white light or fluorescence cystoscopy according to the time from the last BCG instillation. The sensitivity with either modality was 80% or greater at almost all time points following BCG treatment, and no significant differences in sensitivity were observed between either modality at any time point.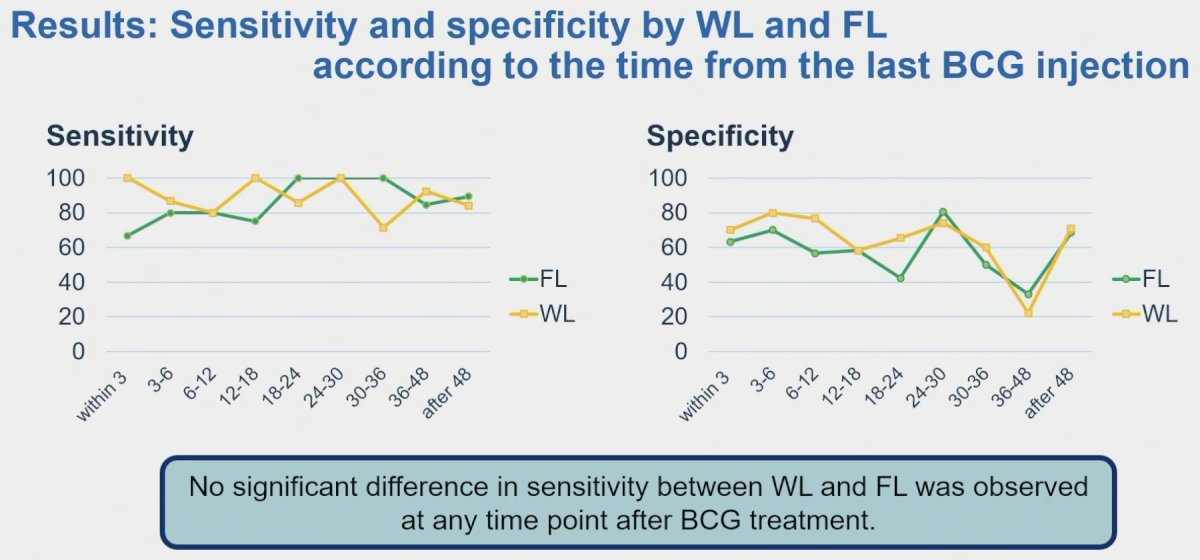
Among 308 lesions resected in patients with prior BCG treatment, 89 (29%) were positive for malignancy. In these patients, use of fluorescence cystoscopy contributed to the diagnosis of 8/19 cancerous lesions (9%).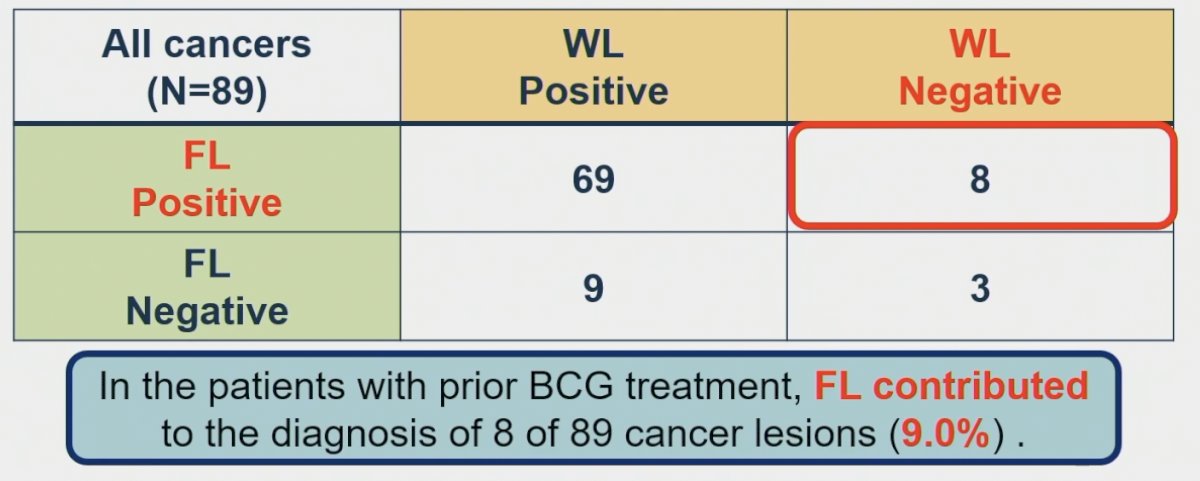
On a patient level, 42/63 patients (67%) were diagnosed with recurrent bladder cancer. Among these 42 patients with recurrent malignancy, fluorescence cystoscopy provided more accurate pathologic diagnosis in only two patients (4.8%).
Dr. Ishikawa concluded that the diagnostic benefit of fluorescence cystoscopy-guided TURBT with 5-ALA appears to be limited in patients with prior BCG treatment, irrespective of the time from the last BCG instillation.
Presented by: Yudai Ishikawa, MD, Department of Urology, Tokyo Medical and Dental University, Bunkyo-ku, Tokyo, Japan.
Written by: Rashid Sayyid, MD, MSc - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, May 3rd - 6th, 2024


