(UroToday.com) The 2024 American Urological Association (AUA) annual meeting featured the AUA-IBCG Bladder Cancer Forum and a series of presentations by Drs. Sia Daneshmand, Seth Lerner, and John Taylor discuss the optimal management of pelvic lymph node dissection for patients during radical cystectomy. As moderator, Dr. Taylor started by highlighting that lymph node involvement is the most significant predictor for mortality, including the number of positive nodes versus lymph node density, and response to therapy. There are several ongoing problems:
- According to the SEER registry, historically 40.3% of patients do not undergo a lymph node dissection, which has improved to 19% more recently
- 20-40% of patients with < pT2N0 disease recur, strongly suggesting there is pathological understaging
- There are no markers to predict presence of nodal disease
- There is a trend towards increasing the regions of dissection
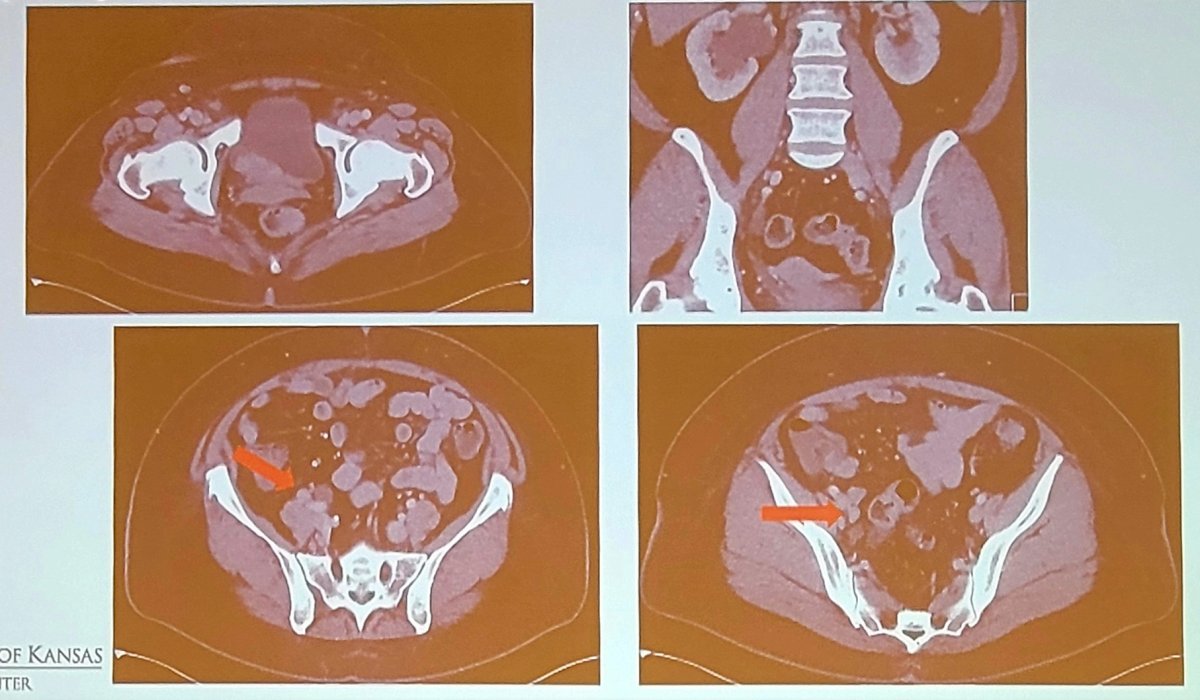
However, both the SWOG S1011 and LEA trials suggest there is no survival benefit for extended pelvic lymph node dissection. Dr. Taylor then discussed a case of a 59-year-old woman with cT3N1/2M0 bladder cancer who has diabetes mellitus with peripheral neuropathy and hearing loss, thus she is not eligible for cisplatin chemotherapy:
Dr. Lerner then took the position of standard lymph node dissection for this patient. The primary objective of SWOG S1011 was to compare disease free survival in patients undergoing radical cystectomy for muscle invasive bladder cancer treated with radical cystectomy and extended pelvic lymph node dissection versus standard pelvic lymph node dissection. Secondary objectives included: overall survival, operative time, post-operative morbidity (from surgery until 90 days after surgery), length of hospital stay, lymph node counts and lymph node density, as well as adjuvant chemotherapy received. The study design for SWOG S1011 is as follows:
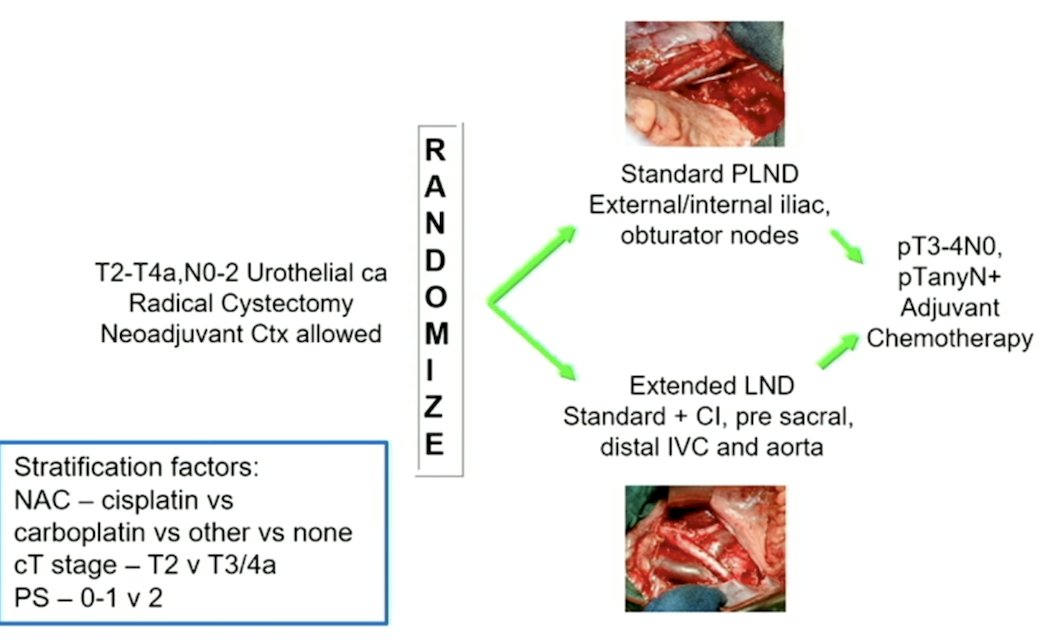
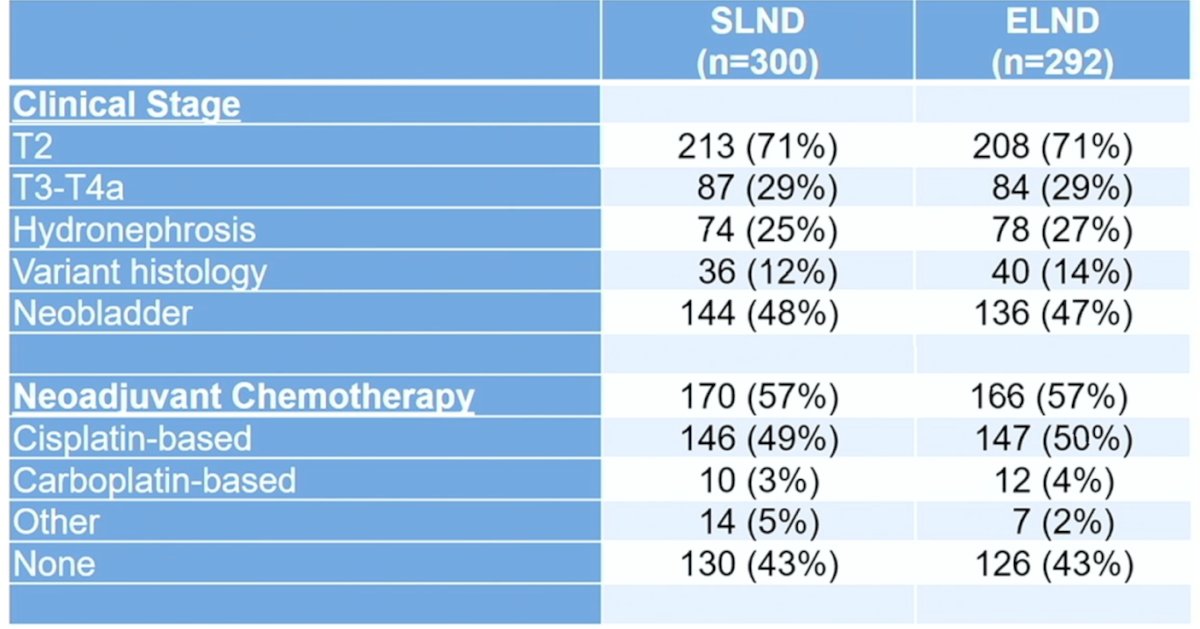
Statistically, assuming a 3-year disease free survival in the standard lymph node group (based on a review of 8 surgical series 2000-2009, including 7,957 patients), there would be 85% power to detect a 10-12% improvement in 3-year disease free survival with extended lymph node dissection (HR 0.72), with a sample size of 564 eligible patients (282 per arm). Assuming a 10% intraoperative ineligibility, the total target accrual was ~620 patients. Ultimately, 592 patients were randomized (n = 300 standard lymph node dissection vs n = 292 extended lymph node dissection), with well balanced clinical stage and neoadjuvant chemotherapy (57% receiving cisplatin-based chemotherapy) variables between the two groups:
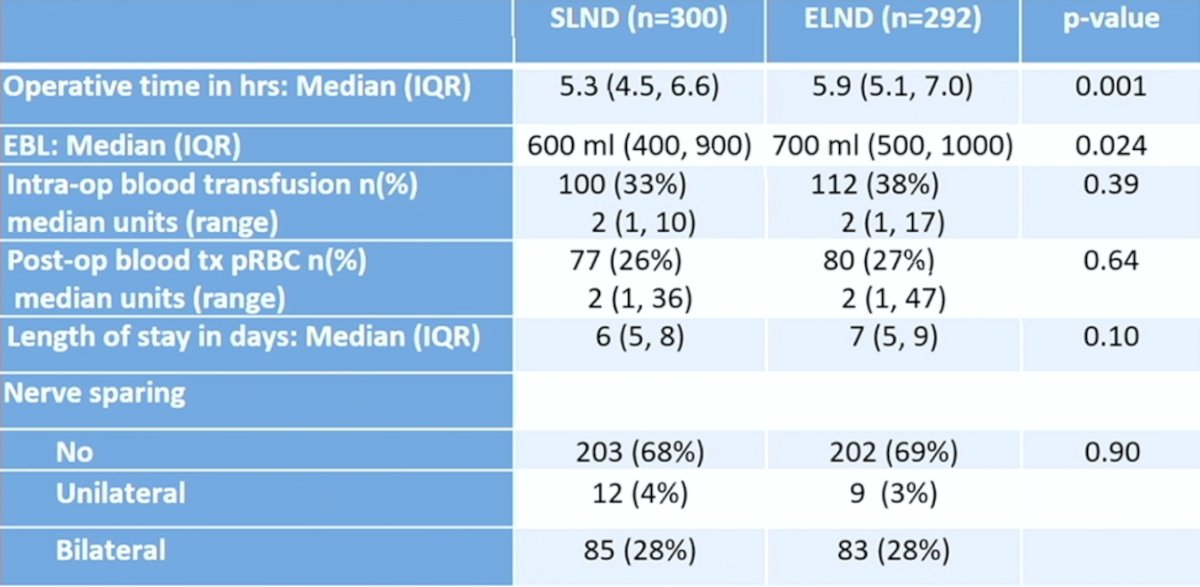
Patients undergoing extended lymph node dissection had a median of 39 nodes removed (range: 15-94) compared to 24 (range: 6-61) for standard lymph node dissection. Furthermore, there was little difference in median number of positive nodes (2, range 1-16 vs 1, range 1-35), between patients receiving extended versus standard lymph node dissection. Additional key findings included a longer median operative time (5.9 hours, IQR 5.1-7.0 vs 5.3 hours, IQR 4.5-6.6; p = 0.001) and more estimated blood loss (700 cc, IQR 500-1000 vs 600 cc, IQR 400-900; p = 0.024) for the extended lymph node dissection group:
This study found that there was no difference in disease free survival (HR 1.10, 95% CI 0.86-1.40) and overall survival (HR 1.13, 95% CI 0.88-1.45) with regards to extended versus standard pelvic lymph node dissection. Importantly, 30-day mortality rate was 30% in the standard lymph node dissection group versus 2.7% in the extended lymph node dissection group, with corresponding 90-day mortality rates of 2.4% vs 6.5%. Higher VTE rates were also noted in the extended lymph node dissection arm:

Dr. Lerner provided the following thoughts as to why there is no added benefit to extended lymph node dissection:
- The assumption of a 3-year 55% disease free survival in the control arm, wherein reality the true 3-year disease free survival was 62%
- The assumption of a 5-year 55% overall survival in the control arm, wherein reality the true 5-year overall survival was 63%
- Completeness of the standard lymph node dissection was quite thorough at 24 nodes, which had a very similar range in the number of positive nodes in both arms
- Disease free survival and overall survival from retrospective data are from the pre-neoadjuvant chemotherapy era, given that 57% of patients had neoadjuvant chemotherapy in this trial, and the prognosis is better in the current era
Dr. Lerner concluded his part of the presentation by discussing SWOG S1011 and no benefit for standard pelvic lymph node dissection with the following take-home messages:
- There was no indication of disease free survival or overall survival benefit for extended lymph node dissection compared to standard lymph node dissection, although salvage lymph node dissection was associated with higher pelvic recurrence in N+ patients
- Extended lymph node dissection was also associated with greater morbidity and higher peri-operative mortality: longer OR time, blood loss, higher number of progression events within 90 days, and higher VTE rate
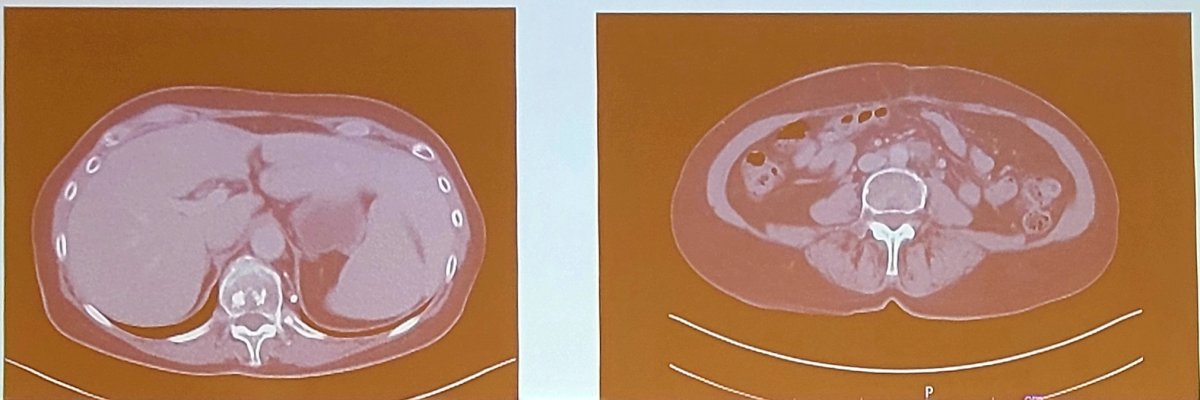
Dr. Daneshmand provided the argument for extended lymph node dissection for this patient. Dr. Daneshmand started by highlighting a case of his own. This patient is a 67-year-old female with cT3 extravesical urothelial carcinoma with extensive tumor necrosis and dystrophic calcifications. She underwent four cycles of neoadjuvant gemcitabine + cisplatin and post-neoadjuvant chemotherapy CT showed mild decrease in the size of the large infiltrative lateral bladder wall mass. She then underwent an anterior pelvic exenteration + standard pelvic lymph node dissection with final pathology showing ypT3aN1M0 urothelial carcinoma with 25% sarcomatoid differentiation and 1 out of 41 positive lymph nodes. One month post-operatively she had a ctDNA of 1.87 MTM/mL and a 2 month post-operative CT scan showed no evidence of disease. A three month post-operative ctDNA showed an increase to 68.52 MTM/mL, and a 4 month post-operative CT scan showed an enlarged left para-aortic and left common iliac lymph nodes above the bifurcation of the common iliac:
Dr. Daneshmand notes that perhaps an extended lymph node dissection would have benefited this patient.
Historically, we know that there is a therapeutic benefit to lymphadenectomy in node negative disease, as well as a therapeutic benefit in node positive disease. Based on large retrospective series, the oncologic benefit of extended pelvic lymph node dissection is likely a 5% 5-year recurrence free survival benefit, which is equal to the benefit derived from neoadjuvant chemotherapy.
In 2011, Dr. Daneshmand was part of a comparative mapping study that showed lymph node dissection technique is more important than lymph node count in identifying nodal metastases in radical cystectomy patients.1 This study assessed 646 patients (439 USC, 207 OHSU), finding 23% had lymph node metastases at time of cystectomy. Although there was a difference in the median per-patient lymph node count between institutions (72 USC, 40 OSHU, p < 0.001), there were no significant interinstitutional differences in the incidence or distribution of positive lymph nodes, which were found in 11% of patients with ≤pT2b and in 44% of patients with ≥pT3a tumors. Among lymph node positive patients, 41% had positive lymph nodes above the common iliac bifurcation. The following figure demonstrates the number of patients with positive lymph nodes at each location:
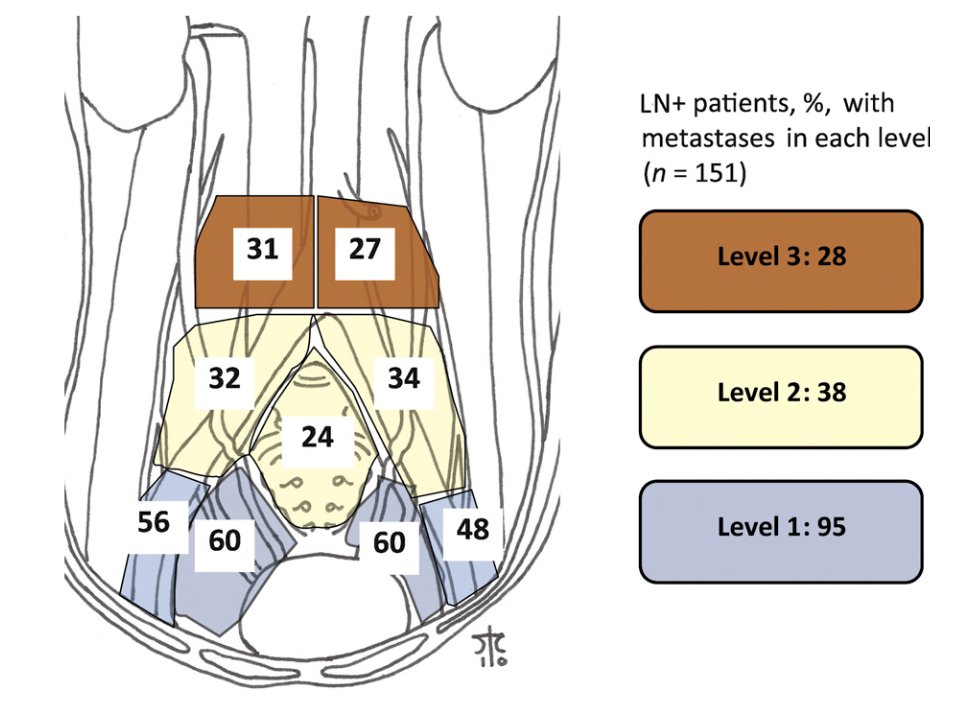
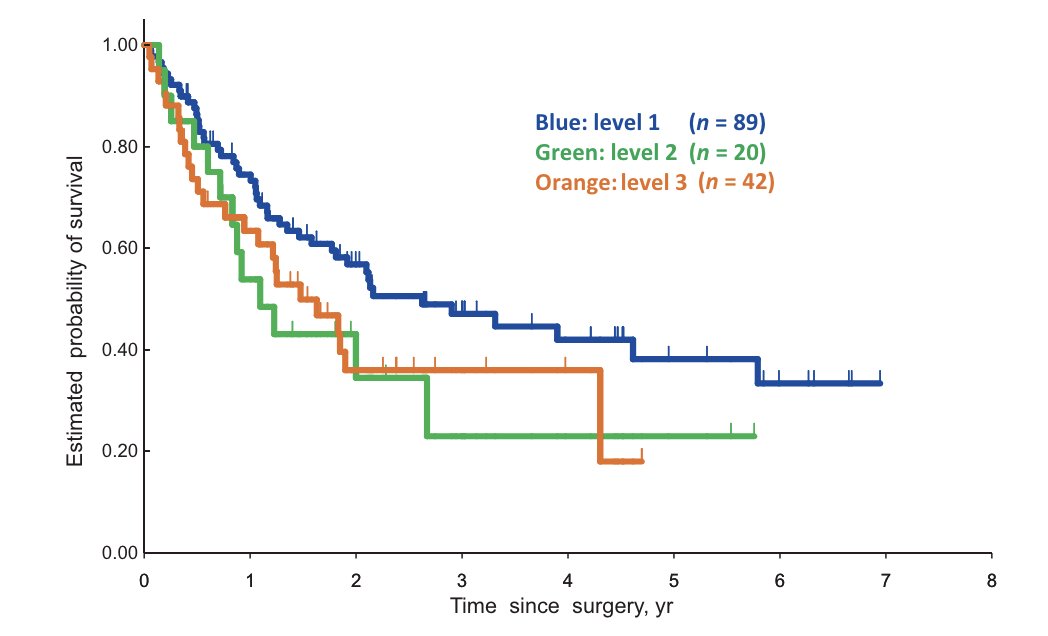
The estimated 5-year recurrence free survival and overall survival rates for lymph node positive patients were 45% and 33%, respectively, and did not differ significantly between institutions. Importantly, the overall survival of lymph node positive patients stratified by the highest level of positive lymph nodes shows differences in survival as follows:
Work from Dr. Daneshmand’s group presented at ASCO 2020 aimed to assess oncological outcomes following radical cystectomy with positive lymph nodes among patients at USC. Among 712 patients (22%) with positive lymph nodes after radical cystectomy, 105 (15%) patients had clinical evidence of lymph node involvement on pre-operative imaging. The 5-year recurrence free survival rates for 1, 2-9 and 10+ positive lymph nodes were 39%, 36% and 16%, respectively (p < 0.001). The 5-year overall survival rates were 45%, 33%, and 14%, respectively (p < 0.001). On multivariable analysis, more than 10 positive lymph nodes pathologic tumor stage >pT2, and neoadjuvant chemotherapy were associated with an increased risk of recurrence and worse overall survival after radical cystectomy.
The AB 25/02 - LEA trial from the Urologic Oncology working group of the German Cancer Society is a prospective, randomized multicenter study to compare an extended versus limited pelvic lymphadenectomy in bladder cancer patients, which was published in 2019 [5]. Among 401 patients with locally resectable T1G3 or muscle-invasive urothelial bladder cancer (T2-T4aM0), 203 were randomized to limited pelvic lymph node dissection and 198 to extended. The median number of dissected nodes was 19 in the limited and 31 in the extended arm. Extended lymph node dissection failed to show superiority over limited lymph node dissection with regard to recurrence free survival (5-year 65% vs 59%; HR 0.84, 95% CI 0.58-1.22; p = 0.36), cancer specific survival (5-year 76% vs 65%; HR 0.70; p = 0.10), and overall survival (5-year 59% vs 50%; HR 0.78; p = 0.12):
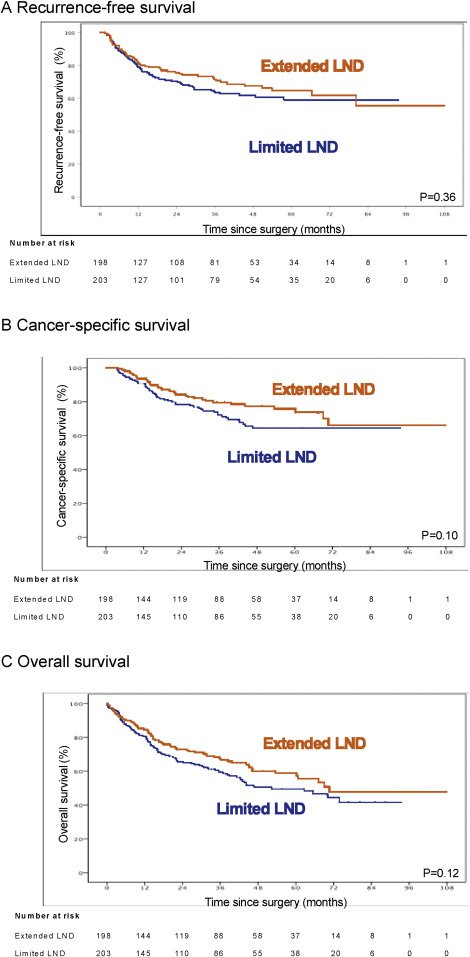
Updated follow-up from this trial (median 58.4 months) has the following outcomes for extended versus standard lymph node dissection:
- 5-year overall survival rate: 57% vs 51%
- 5-year cancer specific survival rate: 76% vs 65%, which is statistically significant
Prospective randomized trials have several unanswered questions:
- Are these trials powered to show a difference in survival of 5-6%?
- What about variant histology?
- What do we do with lymph node involvement near the bifurcation of the common iliac nodes?
- What do we do with lymphadenopathy (cN+) before neoadjuvant chemotherapy?
A new publication from Ben-David et al. [3] found that longitudinal tumor-informed ctDNA predicts disease upstaging and poor prognosis in patients undergoing radical cystectomy. This study assessed 112 patients undergoing radical cystectomy from 2021-2023, whereby ctDNA was detected before radical cystectomy in 59 patients (53%) and was associated with poor recurrence free survival (log-rank p < 0.0001). Additionally, detectable ctDNA before radical cystectomy was associated with poor outcomes regardless of clinical stage (<cT2 vs ≥cT2) and receipt of neoadjuvant therapy. Following definitive therapy, 27 patients with detectable ctDNA had a change to undetectable ctDNA status, the recurrence free survival rates in this group were at 87% at 6 months and 47% at 12 months. Thus, Dr. Daneshmand notes that patients with detectable ctDNA before surgery could gain an additional survival benefit from a more extended pelvic lymph node dissection template.
Dr. Daneshmand concluded his presentation by arguing for a more extensive lymph node dissection with the following take-home messages:
- A “meticulous” template-based lymph node dissection offers the best diagnostic and therapeutic outcomes
- A quality and thorough dissection is more important than lymph node yield and requires skeletonization of the vessels
- This allows removal of the lymphatic tissue, not just lymph nodes, and improves survival as shown in multiple series
- There may still be a role for extended pelvic lymph node dissection for patients with muscle invasive bladder cancer undergoing radical cystectomy
Debaters:
- Seth Lerner, MD, Baylor College of Medicine, Houston, TX
- Sia Daneshmand, MD, USC, Los Angeles, CA
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, May 3rd - 6th, 2024
References:
- Dorin RP, Daneshmand S, Eisenberg MS, et al. Lymph node dissection technique is more important than lymph node count in identifying nodal metastases in radical cystectomy patients: A comparative mapping study. Eur Urol. 2011 Nov;60(5):946-952.
- Gschwend J, Heck MM, Lehmann J, et al. Extended versus limited lymph node dissection in bladder cancer patients undergoing radical cystectomy: Survival Results from a prospective randomized trial. Eur Urol 2019 Apr;75(4):604-611.
- Ben-David R, Tillu N, Cumarasamy S, et al. Longitudinal tumor-informed circulating tumor DNA status predicts disease upstaging and poor prognosis in patients undergoing radical cystectomy. Eur Urol Oncol. 2024 Mar 1 [Epub ahead of print].


