(UroToday.com) The 2024 American Urological Association (AUA) annual meeting featured the AUA-IBCG Bladder Cancer Forum and a series of presentations by Drs. Juan Palou, Paulo Gontero, and Michael Cookson discuss the management of very high risk non-muscle invasive bladder cancer with variant histology. Moderator Dr. Juan Palou started by highlighting that it is important to know when to consider a radical cystectomy in non muscle invasive bladder cancer. Previous work suggests that for cT1 high grade disease, recurrence risk is 42% (95% CI 39-45%), progression risk is 21% (95% CI 18-23%) and cancer specific survival is 87% (95% CI 85-89%). With regards to risk of progression, T1b or T1c substage is arguably the most important risk factor:

It’s important to note that what constitutes high risk tumors, has changed in the last several years with the following table providing a comparison of definitions in 2021 and 2022:

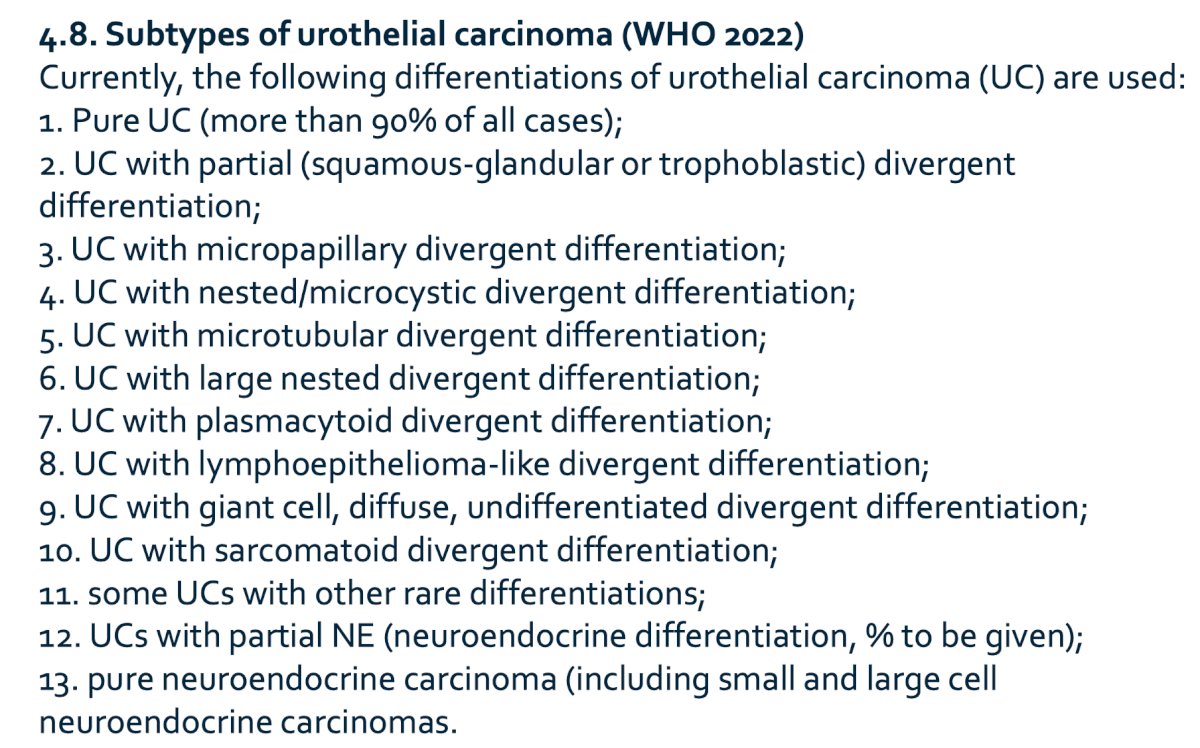
According to the AUA guidelines, variant histology or lymphovascular invasion are key components that make a tumor very high risk, along with BCG unresponsive or prostatic urethral invasion. Furthermore, the following list of subtypes provided by the World Health Organization (WHO) in 2022 are all considered high grade, with the percentage of subtype of prognostic value:
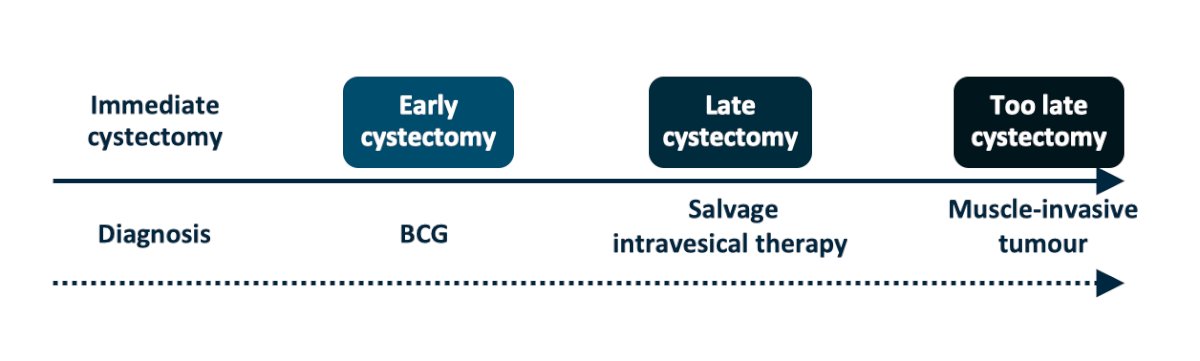
Historical studies suggest that cancer specific survival is worse for muscle invasive disease that has progressed after non muscle invasive bladder cancer versus primary muscle invasive bladder cancer, so the question is when should we do a cystectomy since the likelihood of cure decreases with advancing disease stages:
Dr. Palou then presented a case of a 73-year-old white male with a medical history including hypertension and dyslipidemia. He presented with macroscopic hematuria and underwent a cystoscopy that showed a 2 cm papillary tumor located at the right lateral wall and a 1 cm tumor near the ipsilateral ureteral orifice. A preoperative cytology was positive for high grade urothelial carcinoma and a CT scan showed a 2 cm tumor on the right lateral wall with no hydronephrosis and no lymphadenopathy. His pathology after complete resection was cT1a high grade urothelial carcinoma with 35% plasmacytoid subtype; muscle was present in the sample and multiple biopsies of the bladder were negative for CIS. Dr. Paulo then polled the audience with the following question “For a patient with a 2 cm cT1a (muscle present and uninvolved) with plasmacytoid subtype, how do you proceed?”
- Re-TURBT + BCG: 23%
- BCG: 0%
- Radical cystectomy: 69%
- Neoadjuvant chemotherapy + radical cystectomy: 8%
Dr. Cookson then took the approach that we may consider a role for intravesical therapy. The WHO in 2016 suggested that there are multiple subtypes of urothelial tract tumors, highlighted in the following figure:

According to the 2024 AUA/SUO guidelines, statement 7 suggests “If a bladder sparing approach is being considered in a patient with variant histology, then a clinician should perform a re-staging TURBT within 4-6 weeks of the initial TURBT. (Expert Opinion)” Furthermore, guideline statement 8 states “Due to the high rate of upstaging associated with variant histology, a clinician should consider offering initial radical cystectomy. (Expert Opinion)” When Dr. Cookson dug further into the evidence for this statement, he noted that this is based off of a study of 94 BCG unresponsive patients that did not undergo radical cystectomy, of which only 14 patients had variant histology:1

Dr. Cookson notes that the “best” evidence for immediate cystectomy for micropapillary bladder cancer comes from a 2014 survey among SUO members. Among 118 respondents, 80% considered bladder cancer their primary area of interest. Among them, 78% treat micropapillary bladder cancer differently than conventional urothelial carcinoma, with 81% reporting that they would treat cT1 micropapillary bladder cancer with upfront radical cystectomy. However, the respondents had split opinions regarding the sensitivity of micropapillary bladder cancer to cisplatin-based chemotherapy, which affected the utilization of neoadjuvant chemotherapy in muscle-invasive disease. However, Dr. Cookson emphasized that the problem with surveys is that they are not evidence based medicine, but rather “eminence based medicine” such that some may make the same mistakes with increasing confidence over an impressive number of years.
In the Memorial Sloan Kettering Cancer Center experience with micropapillary bladder cancer was reported in 2014,3 among 36 patients, early radical cystectomy was performed in 15 patients (42%) while 21 (58%) underwent conservative treatment. Over a median follow-up time of 3.1 years (IQR 1.1-5.9), the 5-year cumulative incidence of metastasis was 21% and 34%, respectively, with an absolute difference of 13% (95% CI -23-49, p = 0.90):

The authors concluded that using proper selection criteria, including patient and pathologic factors, certain patients with cT1 micropapillary bladder cancer may be managed conservatively.
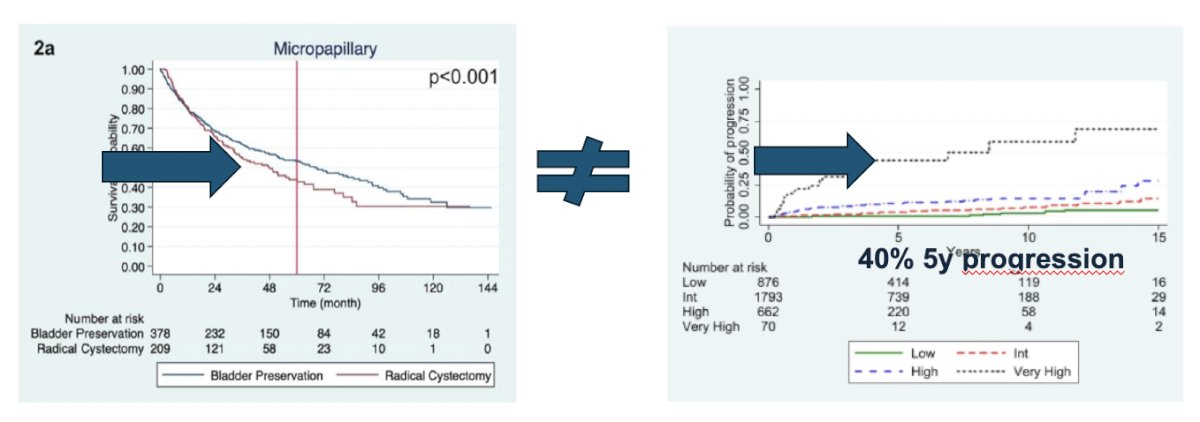
In another study from the EAU Young Academic Urologists committee, they assessed survival outcomes after immediate radical cystectomy versus conservative management with BCG among 119 T1 high-grade micropapillary bladder cancer patients.4 Immediate radical cystectomy and conservative management were performed in 27% and 73% of patients, respectively. Of note, cancer specific mortality (p = 0.50) and overall mortality (p = 0.90) did not differ significantly among patients treated with immediate radical cystectomy versus conservative management:

Overall, 66.7% and 34.5% of patients experienced disease recurrence and disease progression after conservative management, respectively.
Dr. Cookson concluded his portion of the debate by discussing conservative management for variant histology with the following take-home messages:
- Variant histologies are increasingly being recognized in genitourinary pathology reports
- The historical recommendation for radical cystectomy is based more on dogma than on evidence
- There can be strong consideration for bladder preservation for most variants
- There needs to be improved molecular profiles and enhanced awareness amongst pathologists
- We must abide by principles of proper staging, repeat resection, intravesical therapy, and vigilant surveillance
- There must be a call to arms to advance the science with clinical trials that include variant histologies
Next. Dr. Gontero took the position of immediate cystectomy for variant histology patients. He started by emphasizing that divergent pathology subtypes are present in up to 30% of urothelial carcinomas and thus no longer a rare entity. However, they have aggressive features at diagnosis, and unlike pure urothelial carcinoma, 70% are muscle invasive at diagnosis and the remaining is T1, which is clearly a bad pathological variable. The caveats are as follows:
- With these different histological subtypes, are there different outcomes?
- There is generally poor quality of evidence
- Variant histologies are often excluded from trials on new conservative options
In a SEER registry study published in 2021 encompassing 11,000 subtypes, adenocarcinoma, squamous, and endocrine had worse survival than pure urothelial carcinoma. Notably, the survival of other histologies, such as plasmacytoind, are even worse:5

Dr. Gontero emphasized that for micropapillary bladder cancer, some series clearly support the role of early cystectomy:
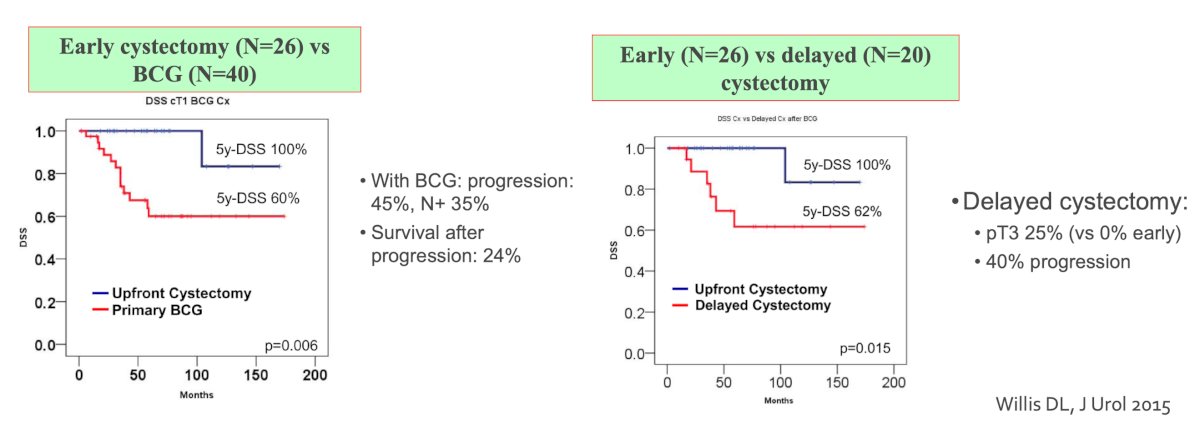
Reassessing data from Lonati and colleagues [4], Dr. Gontero states that these series showing no advantage for radical cystectomy are heavily biased, and unfavorable pathological factors in radical cystectomy patients (ie. more concomitant CIS) likely explain the superiority of BCG. Work from Dursun et al. [6] compared the overall survival outcomes of non-muscle invasive bladder cancer patients with variant histology who underwent radical cystectomy versus bladder preservation therapy among 8,920 patients in the NCDB. Among these patients, 2,450 (27.5%) underwent radical cystectomy, while 6,470 (72.5%) had bladder preservation therapy. When compared with bladder preservation therapy, patients who underwent radical cystectomy had significantly higher 5-year overall survival rates for sarcomatoid (31.9% vs. 23.3%, p < 0.001) neuroendocrine (31% vs. 21.7%, p < 0.001), glandular (44% vs. 41%, p = 0.04) and squamous variants (39.7% vs 19.9%, p< 0.001). This overall survival benefit was not observed with micropapillary variant (43.9% vs. 53.2% p = 0.14). Dr. Gontero notes that when you consider that the 5 year survival rate was 50%, which is much worse than the 40% risk of progression in very high risk pure urothelial non muscle invasive bladder cancer, the problem is not which treatment is the best, but whether each treatment was adequate. In his opinion, it is likely that cystectomy was done too late:
Dr. Gontero highlighted several clinico-pathological features that support immediate radical cystectomy:
- Percent of the variant: focal micropapillary may be better treated with BCG than pure micropapillary
- Concomitant lymphovascular invasion: HR 2.4 for progression on multivariable analysis
- Recurrence after conservative management: at late radical cystectomy – 94% muscle invasive, 20% N+, and 5-year cancer specific mortality rates of 40%
- Upstaging at cystectomy: 73% of subtypes are upstaged versus 53% pure urothelial carcinomas
Dr. Gontero notes that the presented case was plasmacytoid, a rare subtype with aggressive features, for which we merely have radical cystectomy data showing that pT1 is a rare occurrence. The radical cystectomy cure rate is lower than pure urothelial but still 40% can be cured. However, cure rate depends upon the staging and hence from early cysectomy. Thus, the rare occurrence of a T1 of this subtype is a unique chance for cystectomy to be curative.
Dr. Gontero concluded his presentation discussing early cystectomy for variant histologies with the following summary points:
- Subtypes of non muscle invasive bladder cancer are generally urothelial carcinoma at very high risk of progression and death
- The available evidence is of such low quality to be biased in favor of conservative therapy in some series
- There are several hints (pathology, survival) that suggest cystectomy is not performed in a timely fashion
- We need to move from the debate between radical cystectomy and BCG to how we can improve outcomes
- Until then, timely radical cystectomy is the preferred option, especially for the case of plasmacytoid presented
Debaters:
- Michael Cookson, MD, University of Oklahoma, Oklahoma City, OK
- Paolo Gontero, MD, San Giovanni Battista Hospital, Turin, Italy
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, May 3rd - 6th, 2024
Related content: Managing Variant Histology in High-Risk Non-Muscle Invasive Bladder Cancer - Michael Cookson & Paolo Gontero
References:
- Iida K, Miyake M, Murakami K, et al. Bacillus Calmette-Guerin-unresponsive non-muscle invasive bladder cancer outcomes in patients without radical cystectomy. Int J Clin Oncol. 2021;26:2104-2112.
- Willis DL, Flaig TW, Hansel DE, et al. Micropapillary bladder cancer: Current treatment patterns and review of the literature. Urol Oncol. 2014 Aug;32(6):826-832.
- Spaliviero M, Dalbagni G, Bochner BH, et al. Clinical outcome of patients with T1 micropapillary urothelial carcinoma of the bladder. J Urol. 2014 Sep;192(3):702-707.
- Lonati C, Baumeister P, Afferi L, et al. Survival outcomes after immediate radical cystectomy versus conservative management with Bacillus Calmette-Guerin among T1 high-grade micropapillary bladder cancer patients: Results from a multicentre collaboration. Eur Urol Focus. 2022 Sep;8(5):1270-1277.
- Deuker M, Martin T, Stolzenback F, et al. Bladder Cancer: A comparison between non-urothelial variant histology and urothelial carcinoma across all stages and treatment modalities. Clin Genitourin Cancer. 2021 Feb;19(1):60-68.
- Dursun F, Elshabrawy A, Wang H, et al. Histological variants of non-muscle invasive bladder cancer: Survival outcomes of radical cystectomy vs. bladder preservation therapy. Urol Oncol. 2022 Jun;40(6):275.e1-275.e10.


