(UroToday.com) The 2024 American Urological Association (AUA) annual meeting featured the AUA-IBCG Bladder Cancer Forum and a series of presentations by Drs. Sima Porten, Roger Li, and Alexandre Zlotta discuss how much risk patients can tolerate in the BCG unresponsive disease space.
Moderator Dr. Zlotta started with a case presentation of a 72-year-old male with excellent performance status and a medical history of type 2 diabetes who presented with a 3 cm high-grade Ta (grade 3) urothelial carcinoma with CIS, and two small high-grade Ta (grade 2) tumors. He underwent induction BCG x 6 cycles and at his 3-month cystoscopy had no evidence of recurrence. He then underwent 3 cycles of maintenance BCG and at his 6 month cystoscopy had multifocal recurrence at the dome, right, and left lateral walls. A TURBT at this time showed high grade Ta (grade 2) with CIS. Dr. Zlotta then polled the audience with the following question “For BCG unresponsive patients at 6 months with multifocal Ta (grade 2) + CIS, how would you treat?”
- New BCG induction x 6: 23%
- Gemcitabine/Docetaxel: 37%
- Clinical trial: 17%
- Nadofaragene firadenovec: 6%
- Pembrolizumab: 2%
- N-803/BCG: 4%
- Radical cystectomy: 12%
Dr. Zlotta notes that the patient subsequently received a second BCG induction, but at 3 months post-re-induction, he had a high-grade Ta (grade 3) bladder tumor, which was a unique lesion close to the dome of the bladder.
Dr. Porten then discussed that one line of therapy before proceeding with radical cystectomy is reasonable for this patient. She started by emphasizing that if you diagnose a patient with BCG failure, BCG-unresponsive, non-muscle invasive bladder cancer, and they are still clinically non-muscle invasive at the time if they undergo a timely cystectomy, the rates of muscle-invasive disease and nodal metastasis is very low. If you allow those patients to progress to clinically muscle-invasive disease, the rates of extravesical disease are nearly three times higher than those trial patients, and the rate of occult nodal metastasis is five times higher if you allow those patients to progress.
To emphasize her point further, Dr. Porten quoted a paper from her co-debater Dr. Li who in 2019 concluded “We confirm that appropriately defined, BCG-unresponsive patients are more likely to require salvage radical cystectomy (54.5% vs 17.9%, p = 0.002). Moreover, those opting for second-line bladder-sparing therapies are less likely to remain free of tumor recurrence (23% vs 69.2%, p = 0.003):1
There continues to be evolving data in the BCG unresponsive disease space with the following bladder-preserving options currently available, or soon to be available:

What about the next therapy? In many of these trials, inclusion criteria did allow for treatments prior to BCG but not in between BCG and eligible recurrence. Thus, it is unknown how to sequence therapies aside from clinical judgment and patient counseling. Dr. Porten notes that clinical judgment is important here based on other nonmuscle invasive bladder cancer settings:
- Can you fully resect the tumor (location, size/volume)?
- Change in disease characteristics: not all BCG unresponsive disease states are created equal
- High-grade T1 + CIS versus high-grade Ta versus CIS alone (focal vs extensive)
- Cystectomy after one bladder-sparing treatment in a clinical trial: occult nodal metastasis present in 5-10%
- Re-image with CT urogram: with increasing lines of bladder sparing therapy it is necessary to monitor sanctuary/hidden sites, such as upper tract disease (increases from 5-10% to 30%) and involvement of the prostatic urethra
We must also take into account patient-centered factors, assessing their current symptoms such as bladder pain and lower urinary tract symptoms (significant quality of life impairment). Approximately 25-40% of patients have quality of life impairment (sleep, IPSS, pain), and 50% have anxiety and coping issues. Other factors include: (i) distance to travel and treatment intensity, (ii) time off work/family obligations (secondary costs of $100 million annually for nonmuscle invasive bladder cancer), and (ii) cost (25% of patients report financial toxicity).
Dr. Porten concluded by assessing the durability of these next lines of therapy, which is modest at best. Kamat et al.2 performed a systematic review and meta-analysis assessing current and emerging bladder-sparing therapies for nonmuscle invasive bladder cancer after BCG therapy, noting the pooled 12-month response rates were 24% (95% CI 16-32%) for trials with two or more prior BCG courses and 36% (95% CI 25-47%) for those with one or more prior BCG courses. In a subgroup analysis, inclusion of ≥50% of patients with CIS was associated with a lower response. Thus, Dr. Porten again emphasized that timely radical cystectomy while still nonmuscle invasive is better than later after progression.
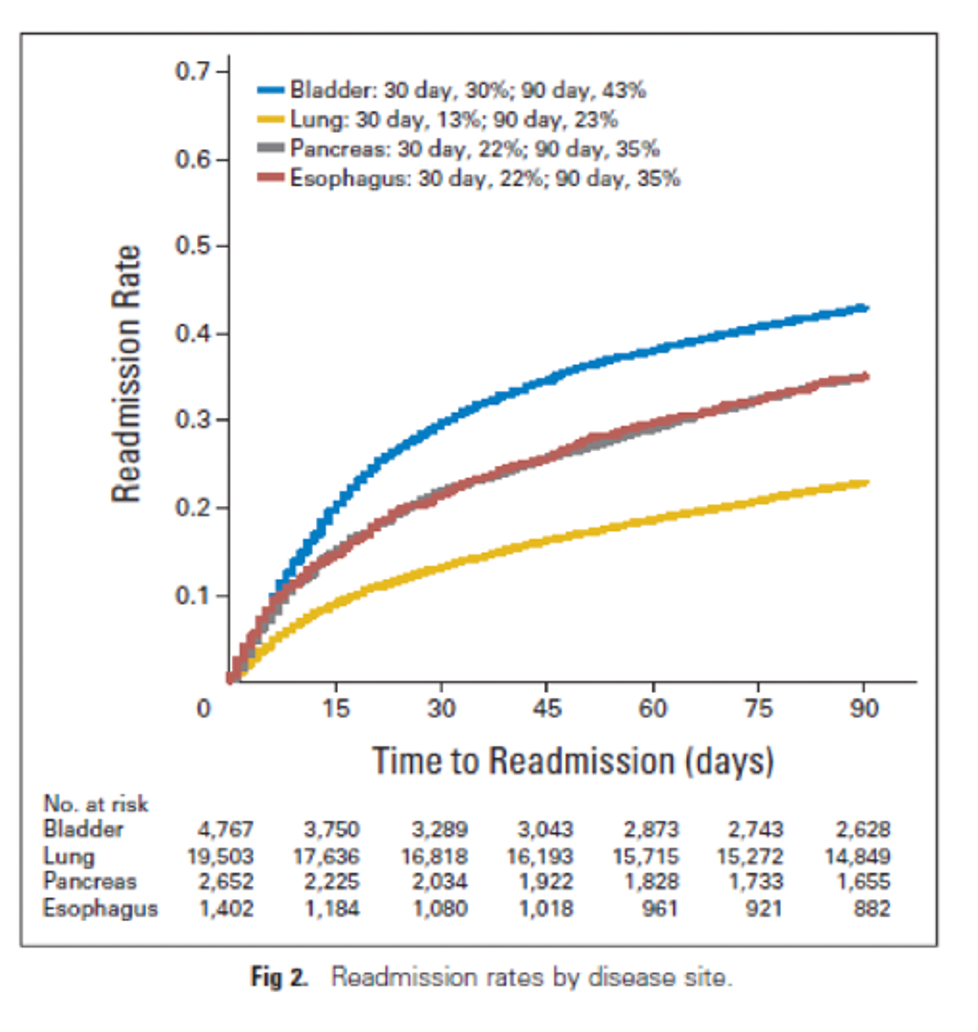
Dr. Li then discussed that sequential therapies should be offered for this patient, specifically highlighting the good, the bad, and the ugly. The ugly is that radical cystectomy is associated with some of the highest surgical complications and readmission rates of any oncology operation performed: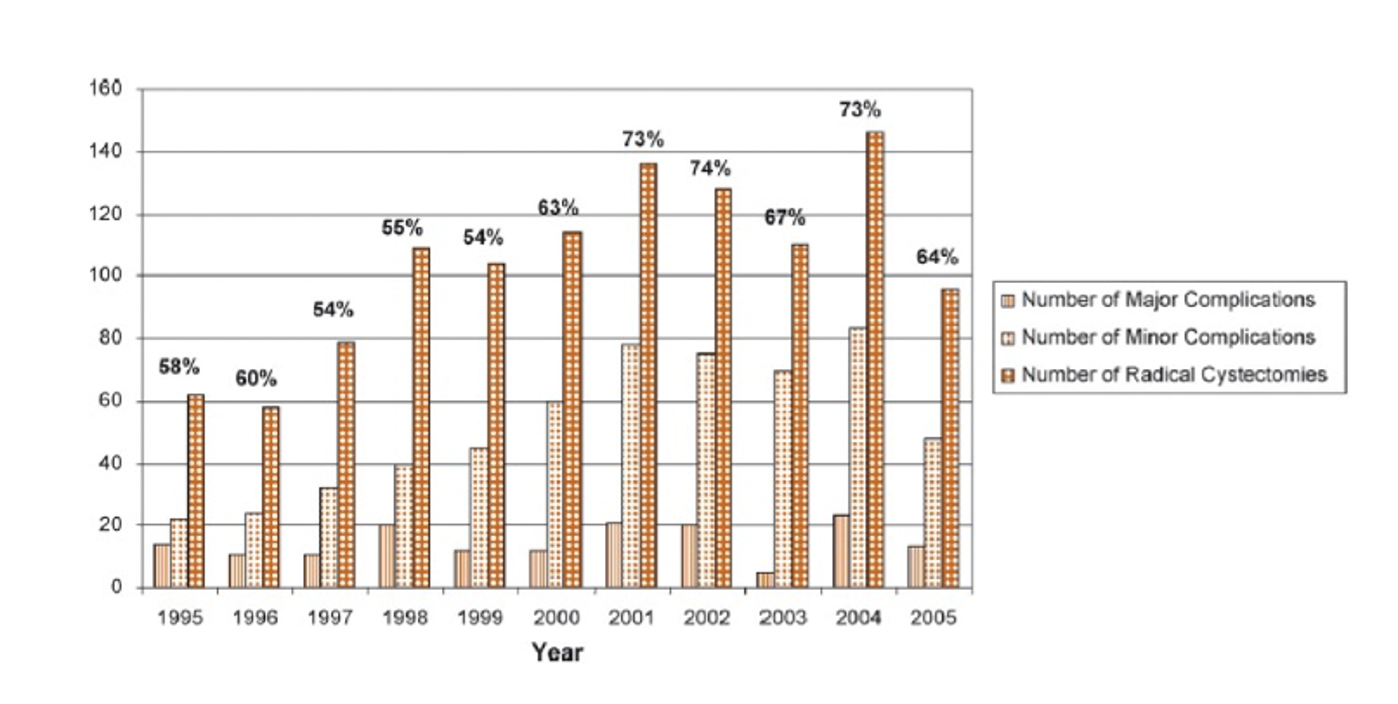
The bad is that patients recovering from radical cystectomy often have major changes to their quality of life during a prolonged recovery of up to 24 months:3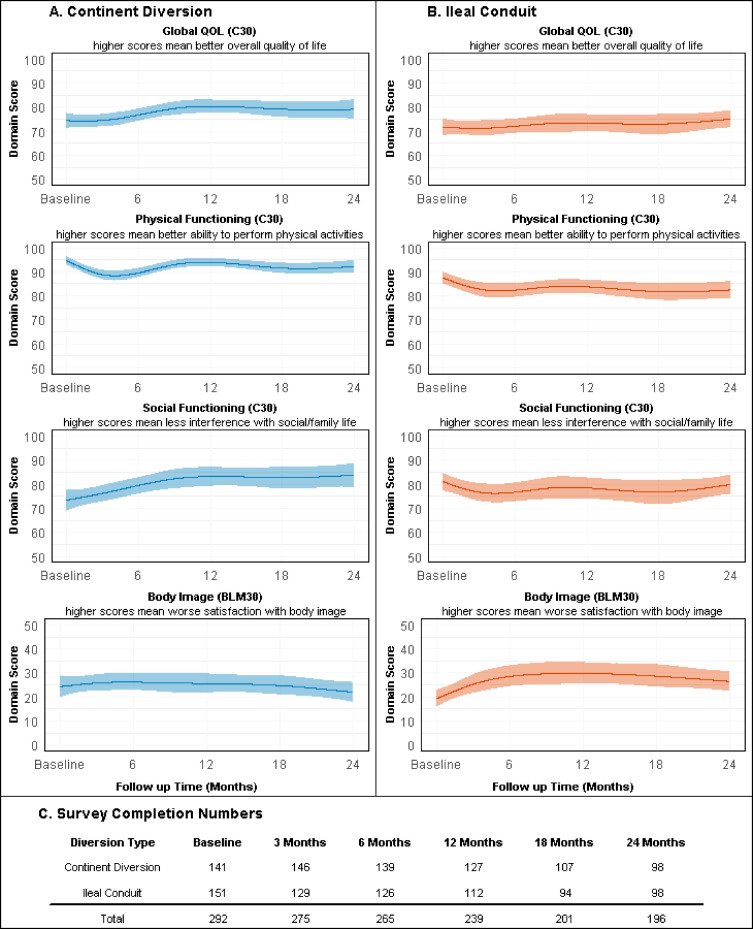
The good? Dr. Li notes that there is not necessarily much good that comes from a radical cystectomy. He then emphasized that bladder-sparing therapy is not as bad as one may think. Work from Tan et al.4 at MD Anderson Cancer Center assessed the long-term survival outcomes of 114 BCG-unresponsive nonmuscle invasive bladder cancer patients treated with bladder-sparing therapy. Over a median follow-up of 71.2 months (IQR 32.6-132.2), there were no significant differences in overall survival (HR 1.40, 95% CI 0.68-2.89, p = 0.40) or cancer-specific survival (HR 0.88, 95% CI 0.22-3.55, p = 0.90) between patients undergoing early radical cystectomy (n = 38) and bladder sparing therapy (n = 76):

Discussing work recently submitted, of which Dr. Li is a co-author, amongst a multi-institutional cohort of 416 patients with BCG unresponsive nonmuscle invasive bladder cancer, 2 patients (0.5%) underwent trimodality therapy, 160 (38.5%) continued with pure BCG (reinduction or additional maintenance), 44 (10.6%) received alternate BCG (reinduction or additional maintenance), and 151 (36.2%) received alterative intravesical agents, most commonly gemcitabine + docetaxel (n = 95, 22.8%). When comparing radical cystectomy to bladder-sparing therapy, there was no difference in progression-free survival (HR 0.88, 95% CI 0.53-1.46), or cancer-specific survival (HR 0.91, 95% CI 0.54-1.53), or overall survival (HR 1.31, 95% CI 0.91-1.90).
Dr. Li concluded his talk discussing bladder-sparing therapies, by emphasizing that the bladder and urine were made for each other and we should not split them apart.
Moderator: Alexandre Zlotta, MD, PhD, FRCSC, Mount Sinai Hospital, Princess Margaret Cancer Centre, Toronto, CanadaDebaters:
- Sima Porten, MD, MPH, Urologic Oncologist, UCSF, San Francisco, CA
- Roger Li, MD, GU Oncologist, Moffitt Cancer Center, Tampa, FL
Written by: Zachary Klaassen, MD, MSc - Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 - Mon, May 6, 2024.
Related content: The Evolving Role of Radical Cystectomy in the Era of Bladder-Sparing Therapies - Sima Porten & Roger Li
References:
- Li R, Tabayoyong WB, Guo CC, et al. Prognostic Implication of the United States Food and Drug Administration-defined BCG-unresponsive disease. Eur Urol. 2019;75(1):8-10.
- Kamat AM, Lerner SP, O’Donnell M, et al. Evidence-based assessment of current and emerging bladder-sparing therapies for non-muscle-invasive bladder cancer after Bacillus Calmette-Guerin Therapy: A systematic review and meta-analysis. Eur Urol Oncol. 2020 Jun;3(3):318-340.
- Clements MB, Atkinson TM, Dalbagni GM, et al. Health-related quality of life for patients undergoing radical cystectomy: Results of a large prospective cohort. Eur Urol. 2022 Mar;81(3):294-304.
- Tan WS, Grajales V, Contieri R, et al. Bladder-sparing treatment in patients with Bacillus Calmette-Guerin-unresponsive non-muscle-invasive bladder cancer: An analysis of long-term survival outcomes. Eur Urol Open Sci. 2023 May 13;53:16-22.


