(UroToday.com) At the AUA 2024 plenary session held on Sunday morning, urologists gathered to delve into the intricacies of bladder pain syndrome (BPS). Dr. William Reynolds opened the discussion, emphasizing the importance of categorizing patients based on their phenotypic characteristics using tools like the Michigan Body Map. He highlighted ongoing advancements in AUA guidelines, particularly categorizing patients into three groups: those with Hunner's lesions, those with localized bladder pain, and those with widespread pain.
Dr. Casey Kowalik then took the podium to explore the management of Hunner's lesions, which are more prevalent in individuals over 50 years old and were first identified in 1914. Characterized by their inflamed and fragile appearance on cystoscopy, these lesions necessitate initial biopsy to exclude cancer, followed by either fulguration or transurethral resection—treatments that show comparable outcomes. Dr. Kowalik discussed additional treatment options including triamcinolone and oral cyclosporine A for resistant cases, while also outlining the significant side effects associated with cyclosporine usage.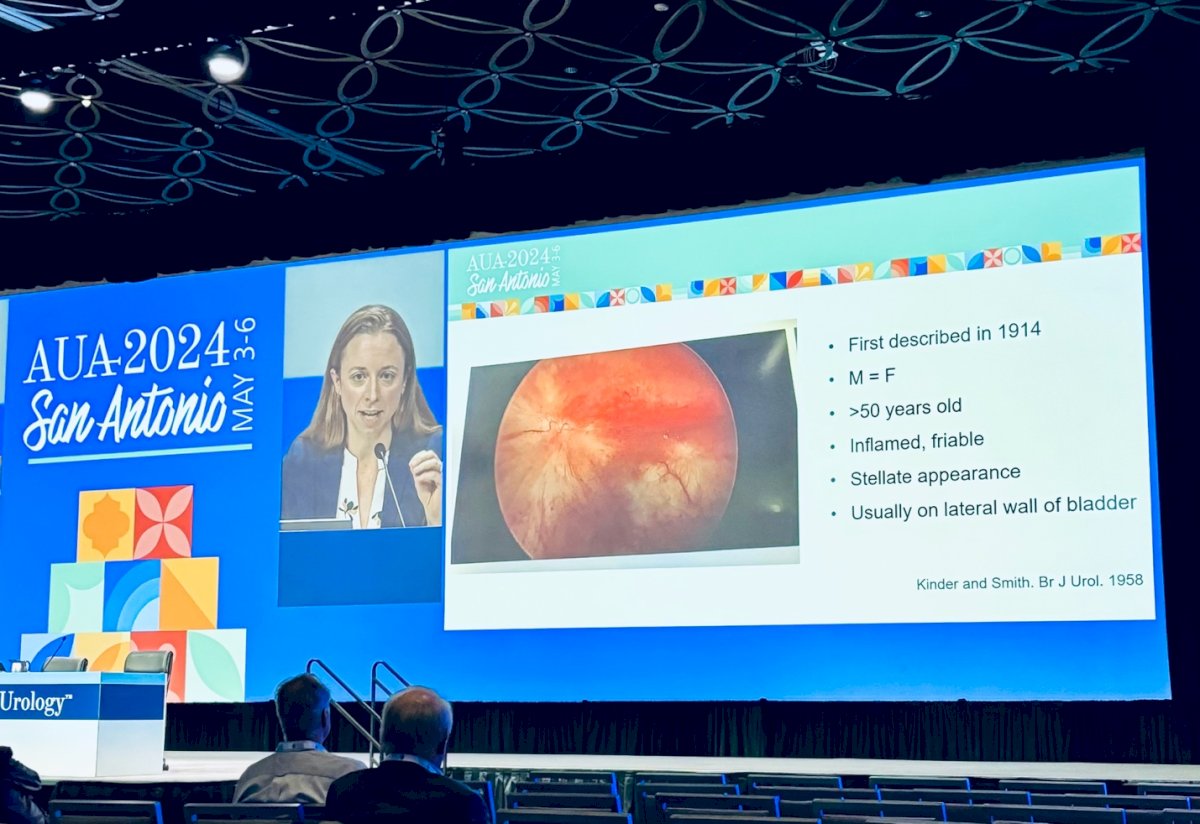
Subsequently, Dr. Amy Dobberfuhl addressed localized bladder and pelvic pain, underscoring the foundational role of the AUA guidelines in managing these conditions. She advocated for a holistic approach incorporating counseling, lifestyle adjustments, and pelvic floor physiotherapy. Dr. Dobberfuhl also reviewed a range of medications, including bladder-specific pentosan polysulfate (PPS), and detailed procedural options like intravesical instillations and hydrodistension, particularly for acute flares.

The session concluded with Dr. William Reynolds summarizing the imperative to tailor treatments to the specific clinical phenotypes of BPS. He reaffirmed the significance of using the AUA guidelines as a reliable resource for managing this complex condition, encouraging continued patient-specific approaches to care.
Presented by:
- William Reynolds, MD, MPH, Vanderbilt University Medical Center, Nashville, TN
- Robert Moldwin, MD, FACS, Smith Institute For Urology, North New Hyde Park, New York
- Casey Kowalik, MD, University of Kansas Health System, Kansas City, KS
- Amy Dobberfuhl, MD, MS, Department of Urology, Stanford University, Stanford, CA
Reference:
- Hanno PM, Burks DA, Clemens JQ, Dmochowski RR, Erickson D, Fitzgerald MP, Forrest JB, Gordon B, Gray M, Mayer RD, Newman D, Nyberg L Jr, Payne CK, Wesselmann U, Faraday MM; Interstitial Cystitis Guidelines Panel of the American Urological Association Education and Research, Inc. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol. 2011 Jun;185(6):2162-70.


