(UroToday.com) Dr. Perry Xu delivered an exemplary presentation on a prospective randomized controlled trial investigating the efficacy of methocarbamol (a skeletal-muscle relaxant) versus oxybutynin (an antimuscarinic/anticholinergic muscle relaxant) for alleviating stent colic. Stent colic poses a significant challenge for patients undergoing surgical management of nephrolithiasis and retrograde intrarenal surgery (RIRS). Despite several existing regimens aimed at mitigating stent-associated pain, the search for an optimal intervention persists. Recognizing this need, Dr. Xu and his team embarked on a comparative analysis of methocarbamol and oxybutynin as potential solutions for relieving stent colic.
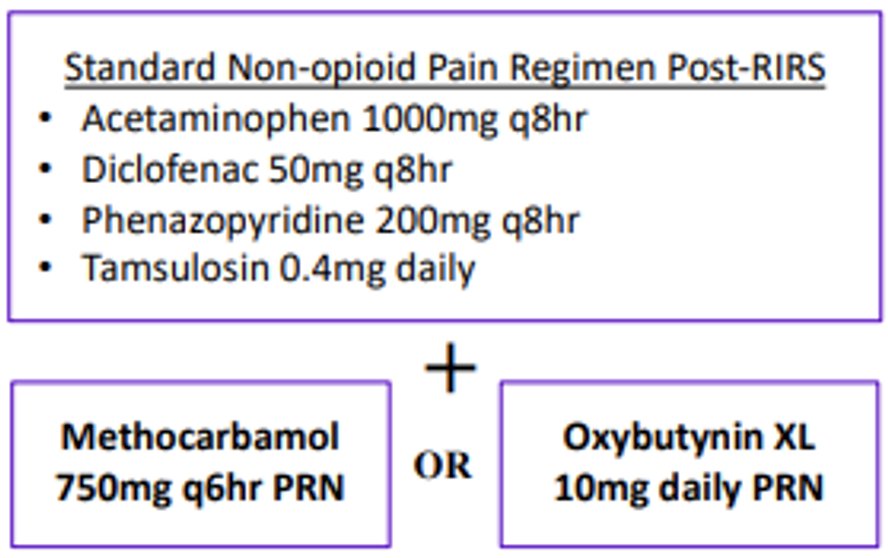
In this investigation, patients undergoing RIRS at a single institution (Northwestern, Chicago) were prospectively randomized into two groups: one receiving methocarbamol 750mg Q6 PRN and the other oxybutynin 10mg XL QHS. Notably, enrolled patients received the study medication in addition to standard postoperative non-narcotic medications, including Acetaminophen 100mg q8hr, Diclofenac 50mg q8hr, Phenazopyridine 200mg q8hr, and Tamsulosin 0.4mg daily.
Exclusion criteria encompassed contradictions, medication allergies, chronic pain history, and opioid dependence. Baseline patient characteristics were obtained preoperatively, with primary outcome measures comprising visual analogue scale (VAS) scores and PROMIS (patient-reported outcomes measurement information system) 3a and 6b scores. Postoperatively, daily surveys were administered to assess VAS and PROMIS scores, alongside additional surveys on emergency room (ER) visits and self-reported complications on postoperative days 15 and 30. Statistical analysis utilized Chi-square tests, Fisher’s exact tests, and student T-tests to compare experimental variables.
Dr. Xu reported a total enrollment of 60 patients, evenly distributed across both groups. Among these patients, several presented with comorbidities including a history of stones, diabetes, and chronic kidney disease (see table below).
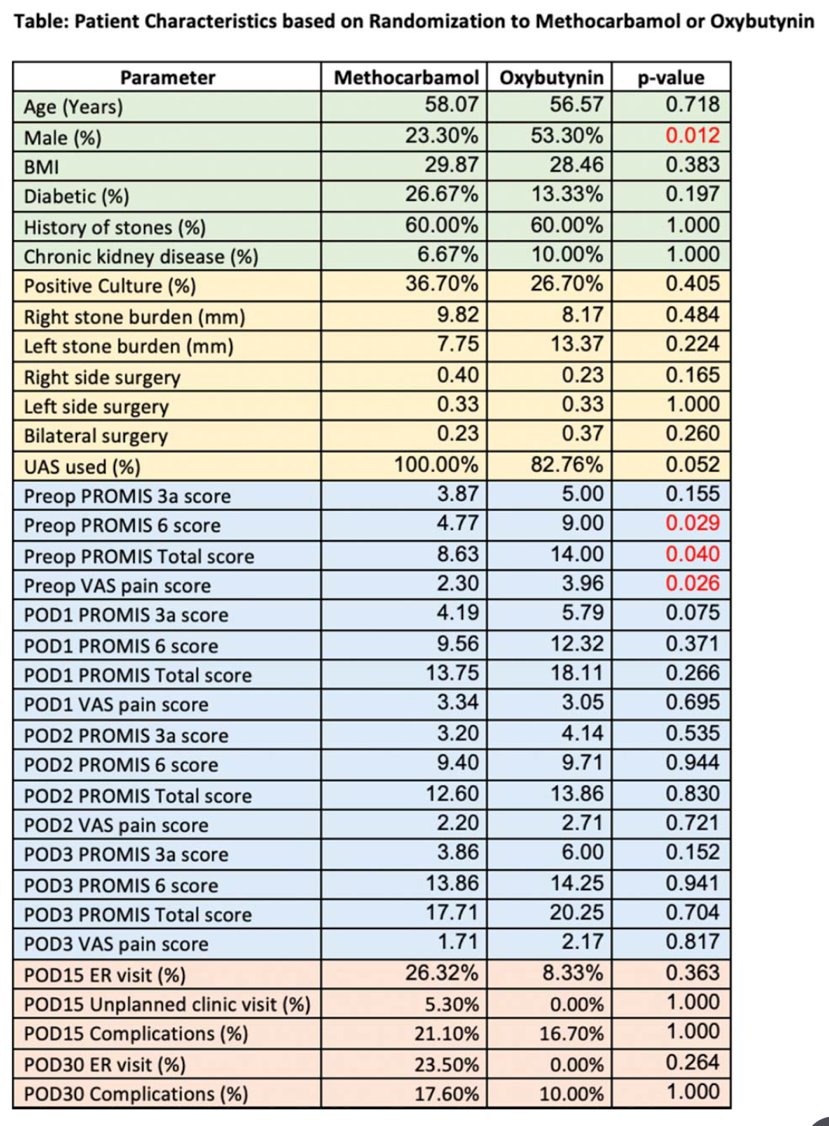
There were no significant differences observed in age and comorbidities between the groups. However, a higher proportion of female patients received methocarbamol compared to oxybutynin (p = 0.012). Analysis of the data presented in the two tables below demonstrated significantly lower total PROMIS and VAS pain scores among methocarbamol recipients compared to oxybutynin recipients (p = 0.04 and p = 0.026, respectively).
No disparities were noted between the 15- and 30-day checkpoints. Ultimately, daily PROMIS and VAS scores did not differ significantly between the two treatment groups.
In conclusion, Dr. Xu emphasized the ongoing challenge of managing stent colic following RIRS. He underscored the importance of tailoring medication selection based on the provider's assessment of each patient's individual needs and tolerability.
During the question-and-answer session, session moderator Dr. Nicole Miller posed an insightful question regarding the rationale behind choosing methocarbamol, given its classification as a skeletal-muscle relaxant. Dr. Xu responded by noting that methocarbamol is utilized in chest, flank, and trauma surgeries as an adjunctive measure, and has documented a reduction in opioid usage in relevant literature. Consequently, Dr. Xu’s team opted to investigate methocarbamol's potential effects on flank muscles, considering the proximity of ureteral stents to this area. When queried about his preferred regimen, Dr. Xu clarified that the study was ongoing but expressed a preference for methocarbamol in combination with other medications such as Tylenol, Flomax, Pyridium, and Diclofenac for patients that are ineligible to be in the study.
An audience member inquired about the study's hypothesis and its impact on patients' quality of life. Dr. Xu elucidated the hypothesis of non-inferiority between the two drugs, citing existing literature supporting oxybutynin's efficacy in stent colic management. Regarding quality of life, Dr. Xu reiterated that they surveyed patients daily to collect data via PROMIS 3a and 6b, which respectively assess pain intensity and interference. Dr. Xu acknowledged that while this method is not flawless for measuring quality of life, PROMIS 6b provided valuable insight into how pain affects patients' daily lives by directly capturing their feedback. In a post-presentation interview, Dr. Xu acknowledged the potential for incorporating additional PROMIS scales to augment the study's comprehensiveness, such as exploring aspects which are difficult to measure like irritative urinary symptoms.
Presented by: Perry Xu, MD, Northwestern University, @perryjxu on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, May 3-6, 2024, San Antonio, Texas
Written by: Seyed Amiryaghoub M. Lavasani, B.A., University of California, Irvine, @amirlavasani_ on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 – Mon, May 6, 2024.


