(UroToday.com) The use of lasers for treating kidney stones, also known as nephrolithiasis, is a hot topic due to recent advancements in laser technology. However, concerns have been raised about high-power lasers that include thulium fiber lasers for kidney stone removal.1 In a well-attended presentation, Dr. Alan Yaghoubian and his team from Mt. Sinai in New York investigated whether high-power Holmium (Ho:YAG) and thulium fiber lasers (TFL) might cause kidney damage during kidney stone removal procedures. This was the first human study to confirm and measure the damage using specific urinary protein markers as indicators of renal damage.
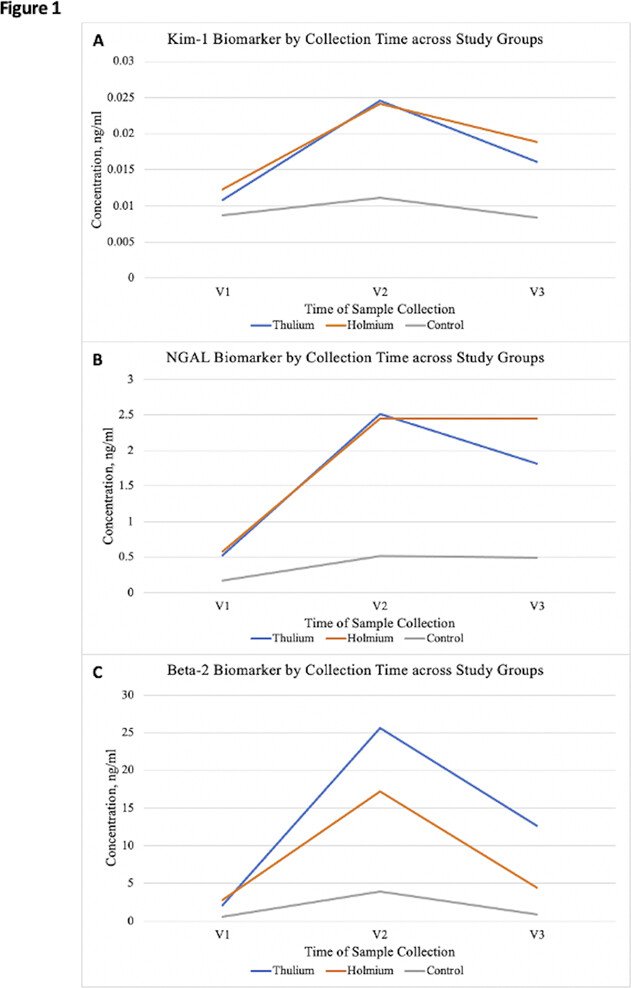
In the randomized controlled trial, patients underwent retrograde intrarenal surgery (RIRS) for unilateral, nonobstructing renal stones (5-20mm total stone burden) and were treated with either 120W Moses 2.0 Ho:YAG or 60W superpulse TFL lasers. A third control group underwent diagnostic ureteroscopy or bladder procedures. Urine samples were collected before the procedure (V1), one hour after (V2), and 10 days after (V3). Researchers analyzed these samples for key biomarkers of kidney injury using the ELISA laboratory technique (Figure 1)
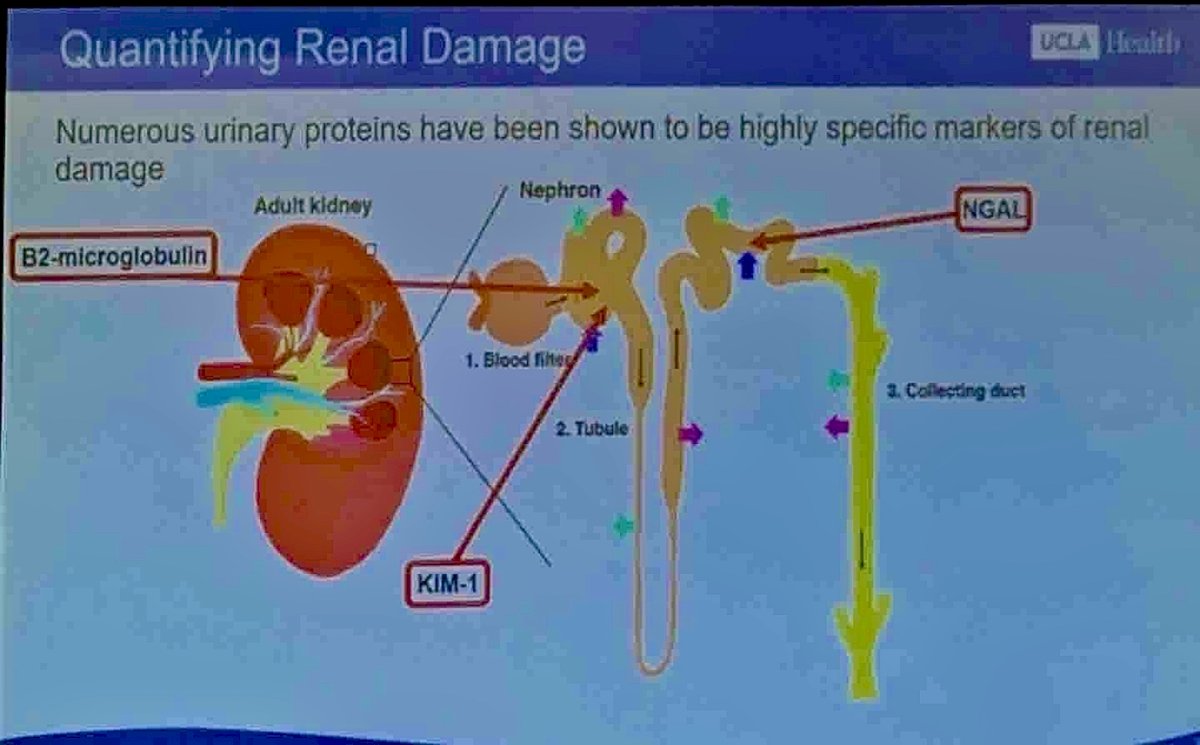
Figure 1. Shows the urinary biomarkers explored and where they are typically found in the nephron.
The researchers maintained consistency by standardizing gravity irrigation (70 cm H2O), using a flexible ureteroscope, and performing stent placement as usual. No ureteral access sheaths were used, and all urologists employed dusting while collecting one stone sample for analysis. This study aimed to mimic "real-world" conditions, allowing physicians to adjust laser settings from 2 to 18 watts as needed and based on their preference.
In total, 104 patients were randomized into either the Ho:YAG or TFL group (52 in each), with five patients serving as controls. Both lasers caused an immediate increase in kidney injury markers post-procedure, but these levels nearly normalized within 10 days (Figure 2). There was no significant difference in the levels of biomarkers or kidney damage between the two laser types. However, the Ho:YAG laser showed a sustained increase in one biomarker (NGAL) even after 10 days, suggesting greater sensitivity to high-energy laser settings.
Overall, the study concluded that both types of lasers can cause kidney damage, but their safety profiles are similar. There were no differences in operative time, stone-free status, laser efficiency, or 30-day complications between the two lasers. Dr. Yaghoubian emphasized the need to be cautious about attributing renal damage solely to heat, renal pressure, or ischemia, as the study could not definitively determine the cause.
During the Q&A session, audience members expressed concerns about renal pressure and operative time and its potential impact on the observed increase in biomarkers. Dr. Yaghoubian acknowledged these valid points and noted that he doesn’t think the 15-minute difference in surgery duration they saw between control and non-control groups is what iss causing the urinary biomarkers. Questions were also raised about whether using an access sheath could lower urinary biomarkers. Dr. Yaghoubian explained that his team does not routinely use ureteral access sheaths, but this approach should be explored to rule out intra-renal pressure as the cause of increased biomarkers.
In conclusion, Dr. Yaghoubian and his team presented a thought-provoking study on the use and safety of high-energy lasers in kidney stone treatment through quantifying renal damage. Further research is needed to fully understand the impact of these lasers on kidney health so that urologist can utilize lasers and minimize renal damage to the patient.
Presented by: Alan Yaghoubian MD, Mt. Sinai, New York, NY
Written by: Paul Piedras, B.S., University of California, Irvine, @piedras_paul on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 - Mon, May 6, 2024.
References:
- Peteinaris A, Tsaturyan A, Bravou V, et al. High-power laser lithotripsy - do we treat or harm? Histological evaluation of temperature effects in an in vivo study with thulium fiber laser. Cent European J Urol. 2023;76(1):44-48. doi:10.5173/ceju.2023.24


