(UroToday.com) Dr. Matthew Sorensen (University of Washington) comprehensively reviewed the evolving approach to managing small stones and fragments. This is essential, especially since all currently available minimally invasive therapies have an increased likelihood of leaving residual stone fragments in place. Although previously referred to as “clinically insignificant”, these urolith fragments serve as a nidus for growth and require retreatment in up to 20% of patients with long-term follow-up data.
The focus on the initial outcomes of the ultrasonic propulsion clinical trial is particularly intriguing. Utilizing non-invasive and non-surgical methods like ultrasonic propulsion to reposition small, asymptomatic residual fragments for easier clearance represents a promising approach. An ultrasound probe, placed on the patient’s skin can be used to sweep fragments towards the ureter from, for example, the lower pole calyx.
The multicenter, randomized controlled trial involving 84 adults with residual stone fragments up to 5 mm in size provides robust data to assess the efficacy of ultrasonic propulsion compared to observation alone. By measuring nephrolithiasis relapse through symptomatic episodes, medical visits, surgeries, or stone growth observed on CT scans, the study addresses important clinical endpoints. Fragment passage and any adverse events were monitored for 21 days or 90 days following the intervention, respectively. Stone growth outcomes were assessed by CT scans at least 90 days after the procedure and continued annually up to a 5-year follow-up period (Figure 1).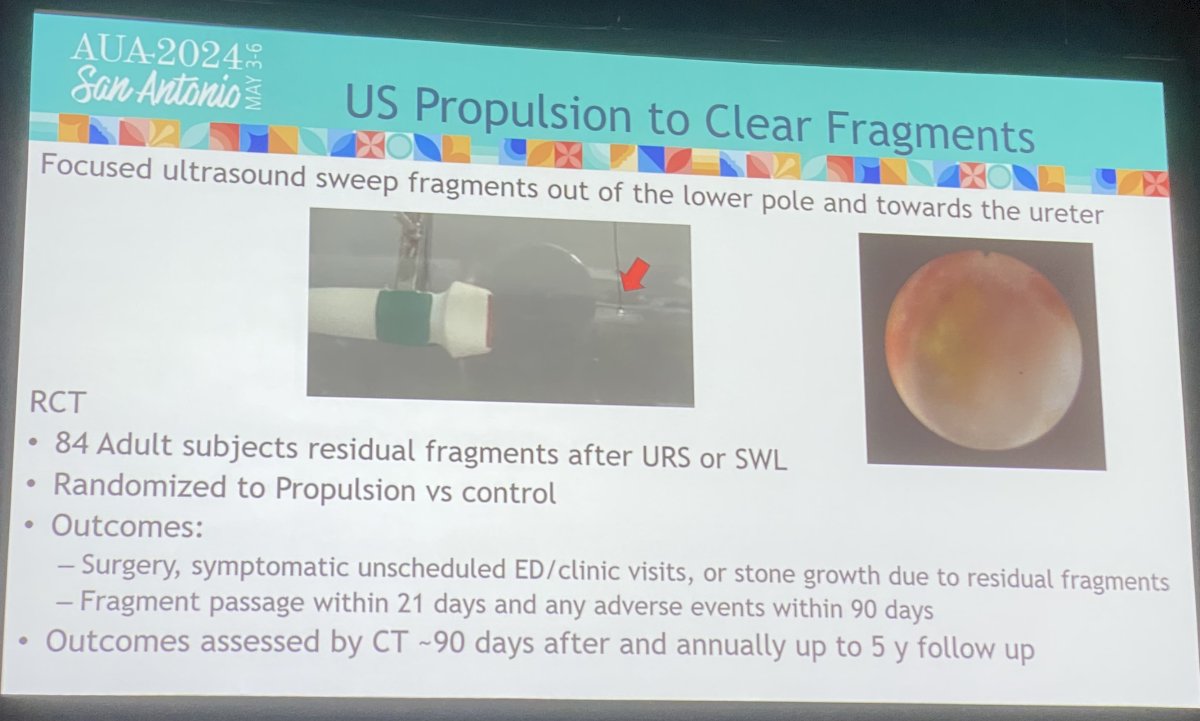
Figure 1. Inclusion criteria for the ultrasonic propulsion randomized clinical trial
Demographic and clinical characteristics were similar (Table 1). After a mean follow-up period of 2.6 years, the risk of relapse was 70% lower in the ultrasonic propulsion group compared to the control group (HR: 0.30; 95% CI: 0.13-0.68). This corresponded to an absolute difference in relapse of 20% vs. 50%, respectively. Moreover, the treatment group had 52% longer time-to-relapse than controls (4.2 vs. 2.8 years, p<0.003, log-rank test) (Figure 2).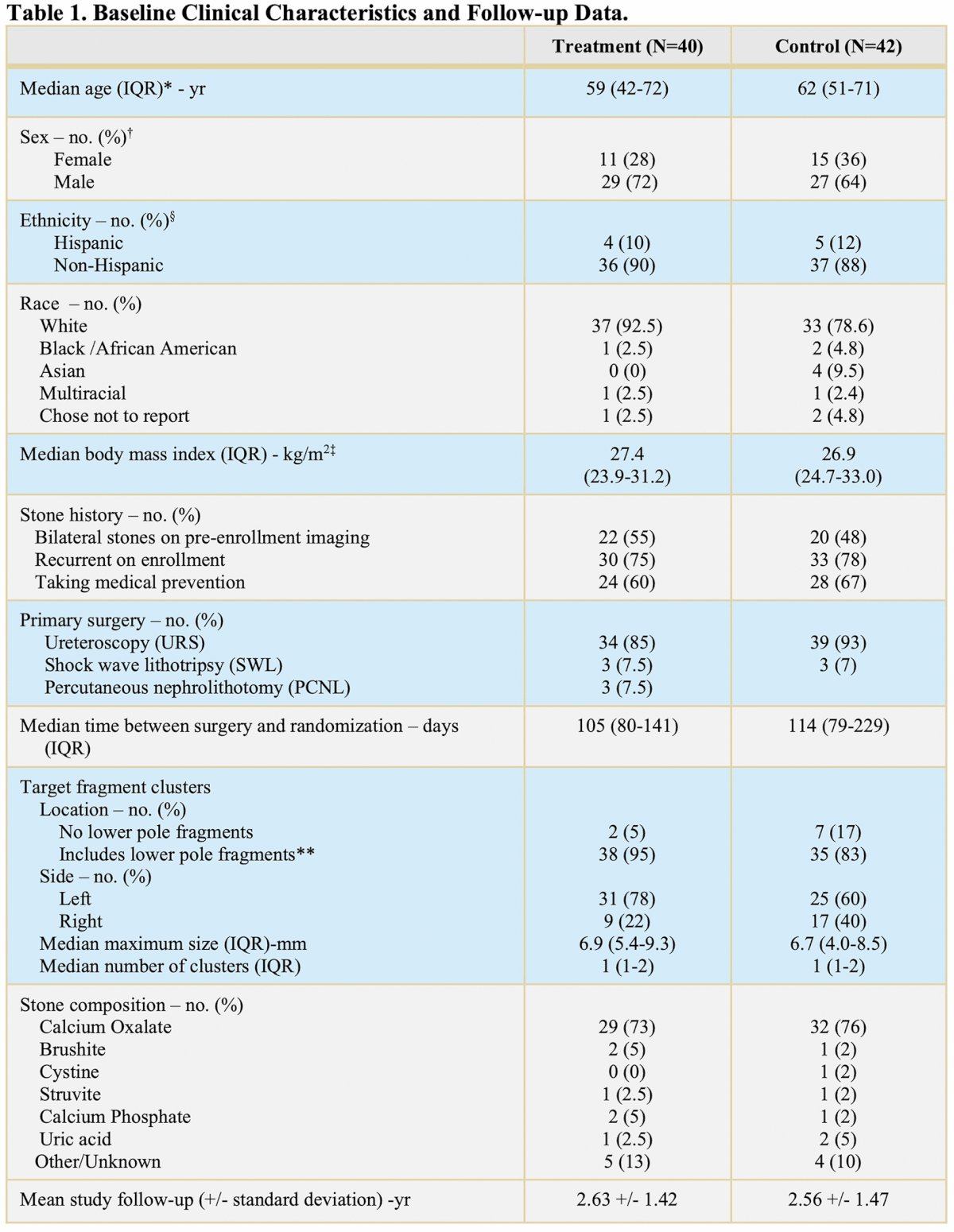
The shaded area represents the 95% confidence interval. Small circles represent censored data. Participant relapse data was censored when participants did not have a relapse before being lost to follow-up or by the end of the follow-up.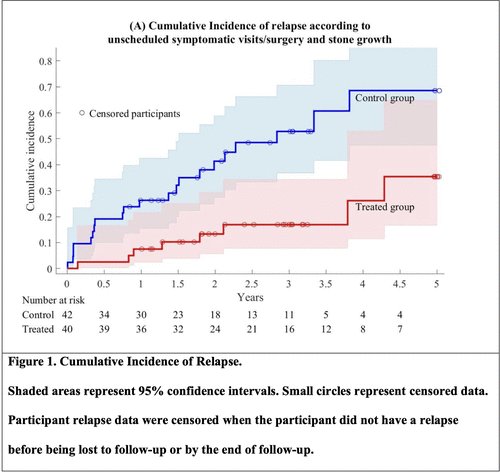
Overall, propulsion-mediated fragment repositioning reduced stone relapse and was well-tolerated in an office-based setting. No medications were needed during any of the procedures. Not surprisingly, the spontaneous stone passage rates within the 3 weeks following ultrasonic propulsion were 12-fold higher in the treatment group (63%) compared to the control (5%). Most of the adverse events were mild and transient: 63% in the treatment group and 40% in the control group.
But what if the same device could help you break down uroliths into smaller fragments as well as facilitate fragment relocation to maximize one’s chances of spontaneous stone passage? This dual functionality could offer a comprehensive solution to both fragment disintegration and repositioning, maximizing the likelihood of spontaneous stone passage while minimizing the need for invasive procedures. Well, the future is way closer than we think with Sonomotion’s ultrasound machine, which facilitates burst wave lithotripsy and ultrasound-promoted fragment relocation (Figure 3). Whether these novel technologies will cause a paradigm shift in small renal stones has yet to be determined, yet the perspective of a novel way of approaching nephrolithiasis, as noted by Dr. Sorensen, is extremely exciting (Figure 4).
Figure 3. Ultrasound-based urolith fragment relocation and burst-wave lithotripsy.
Figure 4. Future Directions
Written by: Andrei D. Cumpanas, MD, University of California Irvine, @andreicumpanas on X during the 2024 American Urological Association (AUA) Annual Meeting, May 3-6, 2024, San Antonio, Texas
References:
- Osman M. Wendt-Nordahl G. Heger K. Michel MS. Alken P. Knoll T. Percutaneous nephrolithotomy with ultrasonography-guided renal access: Experience from over 300 cases. BJU Int. 2005;96:875–878.
- Altunrende F. Tefekli A. Stein RJ, et al. Clinically insignificant residual fragments after percutaneous nephrolithotomy: Medium-term follow-up. J Endourol. 2011;25:941–945.
- Raman JD. Bagrodia A. Gupta A, et al. Natural history of residual fragments following percutaneous nephrostolithotomy. J Urol. 2009;181:1163–1168.
- Rebuck DA. Macejko A. Bhalani V. Ramos P. Nadler RB. The natural history of renal stone fragments following ureteroscopy. Urology. 2011;77:564–568.
- Skolarikos A. Papatsoris AG. Diagnosis and management of postpercutaneous nephrolithotomy residual stone fragments. J Endourol. 2009;23:1751–1755.
- Osman MM. Alfano Y. Kamp S, et al. 5-year-follow-up of patients with clinically insignificant residual fragments after extracorporeal shockwave lithotripsy. Eur Urol. 2005;47:860–864.
- Koh LT. Ng FC. Ng KK. Outcomes of long-term follow-up of patients with conservative management of asymptomatic renal calculi. BJU Int. 2012;109:622–625.
- Preminger GM. Tiselius DG. Assimos D, et al. Guideline for the Management of Ureteral Calculi. 2007. [Mar 21;2013 ]. www.auanet.org/content/clinical-practice-guidelines/clinical-guidelines.cfm?sub=uc
- Sorensen MD, Harper JD, Borofsky MS, Hameed TA, Smoot KJ, Burke BH, Levchak BJ, Williams JC Jr, Bailey MR, Liu Z, Lingeman JE. Removal of Small, Asymptomatic Kidney Stones and Incidence of Relapse. N Engl J Med. 2022 Aug 11;387(6):506-513.
- Sorensen MD, Bailey MR, Hsi RS, Cunitz BW, Simon JC, Wang YN, Dunmire BL, Paun M, Starr F, Lu W, Evan AP, Harper JD. Focused ultrasonic propulsion of kidney stones: review and update of preclinical technology. J Endourol. 2013 Oct;27(10):1183-6.


