(UroToday.com) An expert panel was gathered to discuss second-opinion cases and, the inability to access a tight ureter. Dr. Matthew Bultitude took the stage to introduce to topic at hand. He showed two photographs of patients with tight ureters, one appeared tight, and the other did not, which highlighted that visual assessment is not always possible.
Dr. Bultitude then presented studies that showed ureteral access failure ranged between 6.5% and 20% and the largest study presented showed that younger female patients with more proximal stones might be associated with failed ureteral access. Dr. Bultitude added that there is little guidance for these situations: no guidance from the AUA and EAU guidance of presenting alone.
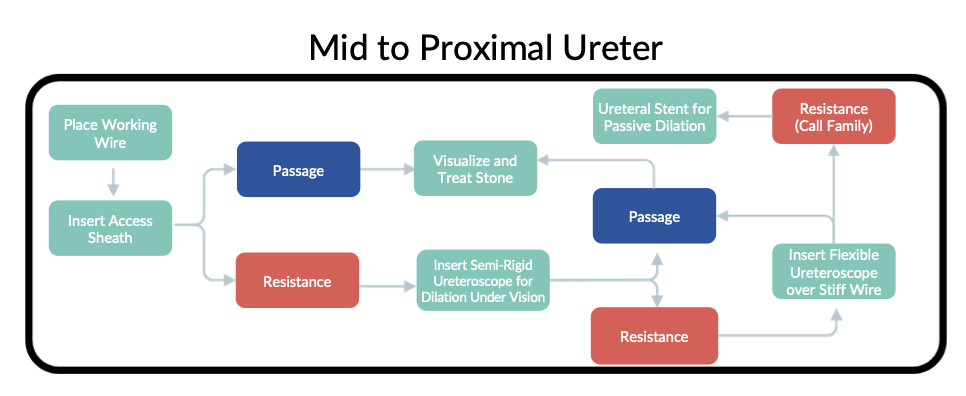
Dr. Bultitude then Introduced the expert panel of Dr. Justin Ziemba and Dr. Julie Riley to present cases and inform the audience about their management strategies. Dr. Ziemba began with a patient who presented with two days of painless gross hematuria. The patient had a CT urogram done, that showed a distal stone with minimal contrast opacification at the ureterovesical junction, which he considered a harbinger of a tight ureter. The patient went to the operating room and a rigid ureteroscope managed to pass the narrowing in the ureter and the stone was treated. Dr. Ziemba next reviewed the tools we have to manage the problem and highlighted that ureteral stent placement was the only passive option. Dr. Ziemba shared two algorithms (shown below) to help guide urologists who encounter this situation.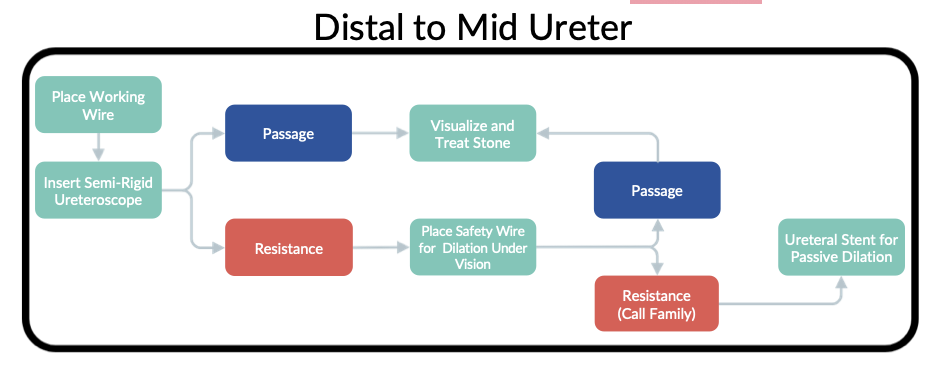
Dr. Riley then took the stage. She presented the case of a patient with a history of multiple ureteral procedures who presented to the emergency department with a lower pole stone, a ureteral stone, severe hydronephrosis in the ipsilateral ureter, and sepsis. The patient was managed with a nephrostomy tube. When the patient returned to the OR for definitive management, the ureteral stone was no longer present, but the ureter could not be accessed due to a narrowing found on retrograde pyelogram and endoscopy. It was known that this patient wanted to avoid multiple procedures, so Dr. Riley used a balloon dilator to allow her to advance an access sheath and treat the lower pole stone. A stent was then placed for two weeks.
Dr. Riley then presented data to further explore the idea of using balloon dilation to access the tight ureter. She informed the audience that in the case of short strictures (< 2 cm), balloon dilation is safe and effective: the success rate was 89% and, despite an 8% chance of perforation, the stricture rate is only 1%. She cautioned that the data is limited, and compliance of the individual ureter is variable by location but in the appropriate patient, benefits include avoidance of multiple procedures and stents, reduction of cost, and maximizing the OR schedule. Dr. Riley ended by providing her algorithm for managing a tight ureter noting that when she does balloon dilate, she ensures the narrowing is short, and uses a 16 Fr balloon inflated to 20 atm for three minutes.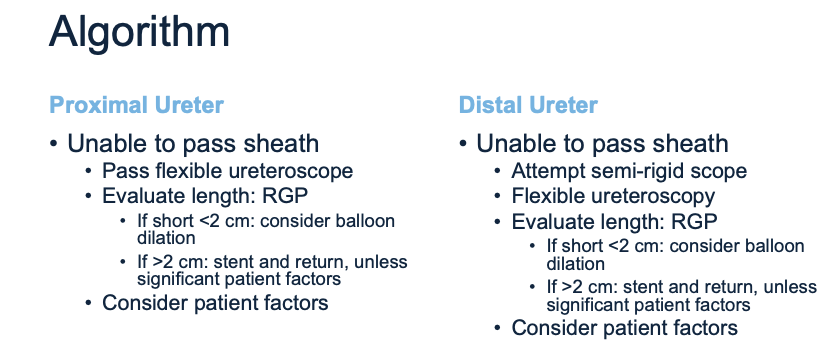
The session concluded by Dr. Bultitude exploring up some provocative questions with the panel as well as referring to a survey of over 200 urologists that he conducted in the UK. In terms of consent, both panelists informed the patient that access via the ureter might not be immediately possible but that the stone would eventually be treated. All on the panel left a stent in place for one to two weeks to dilate the ureter, which mirrors EAU guidelines. Finally, Dr. Bultitude was curious about the use of alpha-blockers before ureteroscopy to aid access. Dr. Riley believed that it was anecdotally helpful and Dr. Ziemba did not routinely prescribe it. Of note, in the UK survey, almost no urologist prescribes alpha-blockers, and Dr. Bultitude cautioned that the meta-analyses that show efficacy could be biased. Overall, this panel provided insight into managing the tight ureter as well as a much-needed framework for urologists to consider in the abscess of guidelines.
- Matthew Bultitude, MD, FRCS (Urol) (Moderator), Consultant Urological Surgeon, Clinical Director, Transplantation, Renal and Urology, Guy’s and St. Thomas’ Hospital, London, England
- Justin Ziemba, MD MSEd, Assistant Professor of Urology in Surgery, Hospital of the University of Pennsylvania, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA
- Julie Riley, MD, FACS, Hal Reed Black Endowed Professor and Chair, University of Arkansas for Medical Sciences, Little Rock, AR


