(UroToday.com) In this edition of the State-of-the-Art lecture series, Dr. Bodo Knudsen provided an extensive overview of the progression and future prospects of laser lithotripsy technologies in endourology. His presentation traced the historical advancements in this field, discussed the current state of the technology, and speculated on future directions. Dr. Knudsen's insights offer a comprehensive guide to both the capabilities and limitations of laser technologies used in the treatment of urinary tract stones.
The introduction of the Holmium:YAG (Ho:YAG) laser in the early 1990s marked a significant milestone in urological surgery. This laser technology is capable of fragmenting all types of urinary stones and offers applications in soft tissue surgery. Its features include short pulse durations and the use of reusable and economical silica laser fibers. Over the years, studies, such as those conducted in 2005 by Dr. Ralph Clayman’s group, have explored the relationship between pulse duration and bubble dynamics, leading to optimized settings that reduce retropulsion—a common challenge in stone fragmentation (Figure 1).1
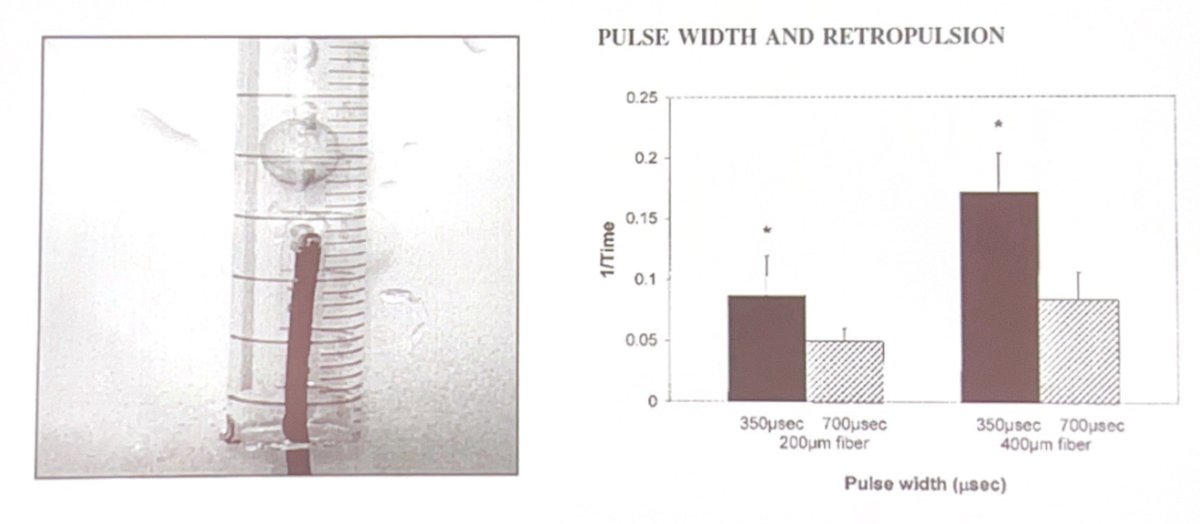
Figure 1. Longer Ho:YAG laser pulse width is associated with greater retropulsion in vitro.
Furthermore, technologies like the Lumenis "Moses" mode and similar innovations from other companies have sought to improve the efficiency of stone fragmentation while minimizing retropulsion and laser fiber burnback.2 However, these advanced modes also come with higher costs that may not always justify the time savings in practical settings.3 Dr. Knudsen posed an important question regarding whether we have reached a technological ceiling with the Ho:YAG laser. He highlighted several limitations, including the need for special electrical outlets due to high power requirements, the susceptibility of complex systems to breakdowns, and the interference of the laser's operation noise with communication in the operating room. Furthermore, the multimodal spatial beam profile of the Ho:YAG laser imposes restrictions on the minimum size of the fiber that can be used.
The introduction of the Thulium Fiber Laser (TFL) in 2019 presented a quieter, more robust alternative capable of using smaller fibers, addressing some of the limitations faced by the Ho:YAG laser. While there was initial excitement over its high-frequency capabilities, subsequent clinical studies have indicated that lower frequencies often yield better efficiencies, particularly in delicate areas like the ureter, due to concerns over heat damage.4,5

Figure 2. Dr. Knudsen illustrates the initial excitement about high frequency capability of TFL with this case capture. “If you can deliver more pulses in the same amount of time – even better dusting?”
Certainly, the TFL offers many advantages, but its limitations include a short pulse duration that is still longer than the long pulse of the Ho:YAG, resulting in lower peak power and less effective stone fragmentation. Discussing future directions, Dr. Knudsen highlighted the TM:YAG laser, which hopes to combine the best features of both Ho:YAG and TFL lasers with lower peak power and longer pulse duration (Figure 3)6. This emerging technology represents a hopeful advancement in the field of endourology.
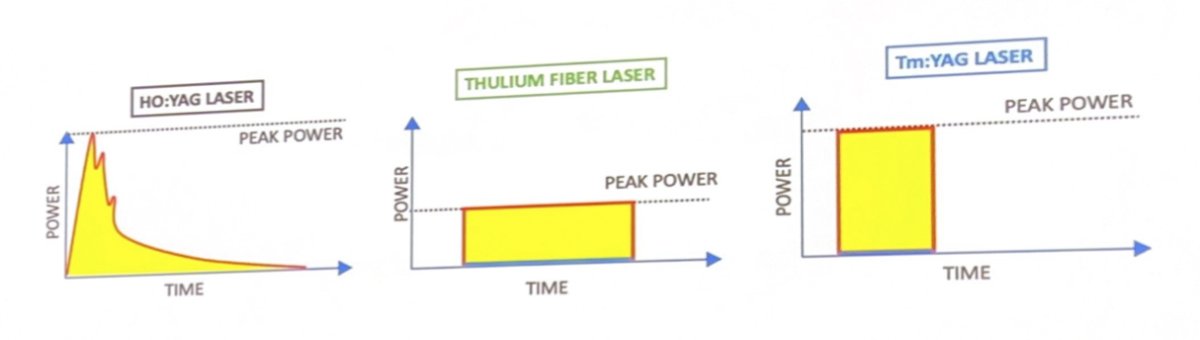
Figure 3. High peak pressure associated with Ho:YAG laser, longer pulse associated with TFL, and “best of both worlds” TM:YAG.
Dr. Knudsen concluded his lecture by emphasizing the responsibility of urologists to optimize the use of existing technologies while being mindful of safety and patient outcomes, leaving us with the words of his fellowship mentor, Dr. John Denstedt: “Think about what we put out into the world and do it in a manner that is safe and thoughtful and improves the lives of our patients”.
Presented by: Bodo Knudsen, MD, Ohio State University Department of Urology
Written by: Brandon Camp, MS3, University of California Irvine School of Medicine, @brandon_camp on X (formerly Twitter) during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 - Mon, May 6, 2024.
References:
- Finley DS, Petersen J, Abdelshehid C, et al. Effect of holmium:YAG laser pulse width on lithotripsy retropulsion in vitro. J Endourol. 2005;19(8):1041-1044. doi:10.1089/end.2005.19.1041.
- Ibrahim A, Elhilali MM, Fahmy N, Carrier S, Andonian S. Double-Blinded Prospective Randomized Clinical Trial Comparing Regular and Moses Modes of Holmium Laser Lithotripsy. J Endourol. 2020;34(5):624-628. doi:10.1089/end.2019.0695.
- Stern KL, Monga M. The Moses holmium system - time is money. Can J Urol. 2018;25(3):9313-9316.
- Molina WR, Carrera RV, Chew BH, Knudsen BE. Temperature rise during ureteral laser lithotripsy: comparison of super pulse thulium fiber laser (SPTF) vs high power 120 W holmium-YAG laser (Ho:YAG). World J Urol. 2021;39(10):3951-3956. doi:10.1007/s00345-021-03619-3.
- Aldoukhi AH, Black KM, Hall TL, Roberts WW, Ghani KR. Frequency Threshold for Ablation During Holmium Laser Lithotripsy: How High Can You Go?. J Endourol. 2020;34(10):1075-1081. doi:10.1089/end.2020.0149.
- Chicaud M, Corrales M, Kutchukian S, et al. Thulium:YAG laser: a good compromise between holmium:YAG and thulium fiber laser for endoscopic lithotripsy? A narrative review. World J Urol. 2023;41(12):3437-3447. doi:10.1007/s00345-023-04679-3.


