(UroToday.com) When it comes to kidney cancer, there are several types, papillary renal cell carcinoma (pRCC) and clear cell renal carcinoma (ccRCC). These cancer types are named based on their characteristics. For pRCC the tumor grows in finger like projections where ccRCC is characterized due to its high lipid content and is typically more aggressive than other subtypes as it is more likely to metastasize.1 Both types are treated with similar approaches such as surgery, targeted therapy, immunotherapy or chemotherapy. Even as we continue to learn about how to treat renal cancer, little is still known about the cells, molecules, and blood vessels that surround the tumors, also known as the tumor immune microenvironment (TIME). Dr. Mitchell Hayes and his team at OHSU and Moffett Cancer Center are among the few researchers exploring the tumor immune microenvironment (TIME) of kidney cancer, offering potential new insights for treatment.
Dr. Hayes and his team used advanced techniques to study tumor samples from patients with localized RCC. They performed multiplex immunofluorescence (mIF), a technique to simultaneously visualize multiple proteins or antigens. mIF was used on tumor specimens, focusing on selected regions of interest to evaluate different parts of the tumor, such as the tumor itself, the surrounding stroma, and areas where the tumor and stroma meet (Figure 1). The team used two different panels of antibodies to identify markers for T cells, B cells, and macrophages. They then compared these markers and their distribution in both pRCC and ccRCC, as well as between early and advanced stages of pRCC. The researchers also used a spatial molecular imaging (SMI) platform, which analyzes specific genetic transcripts, to validate their findings. By quantifying cell clustering and conducting statistical analyses, they gained a deeper understanding of the immune environment in RCC (Figures 2,3, and 4)
By examining tumor samples, researchers found that pRCC has fewer immune cells, particularly T cells and macrophages, compared to ccRCC. Despite this lower count, the study revealed a higher concentration, or clustering, of macrophages in the pRCC tumors. Moreover, the study showed that as pRCC progresses to more advanced stages, there is an increase in CD8+ T cells and a decrease in certain macrophage clusters, suggesting a possible link between the immune environment and the severity of cancer. These findings offer new insights into the differences between pRCC and ccRCC, which could lead to a better understanding and treatment of kidney cancer in the future.
At the end of his presentation, the moderators asked Dr. Hayes if he was able to test and find differences in the genotype of different pRCC subtypes (I and II) to which he answered that they were able to test the genotypes of the two different subtypes, but their focus was more on global differences between pRCC and ccRCC as a potential use for future biomarkers. Another moderator asked Dr. Hayes what he thinks is going on with the “foamy” macrophages and if this is a sign of activation. Dr. Hayes responded with “…our suspicion is that they have some sort of interaction with T-cells, inhibiting them in some way” and proceeded to say that further research needs to be done to make a conclusion about these macrophages.
Dr. Hayes delivered an impressive presentation that showcased his deep understanding of a complex topic. His striking visuals illustrated the diversity of immune cells in renal cell carcinoma and how they are arranged within the tumor. The study overall highlighted the advances made in genetic sequencing and visualizing molecules at the cellular level for cancer.

Figure 1 Shows mIF is and how the different cells are color coded within the tumor.

Figure 2. technique and results from using spatial transcriptomic through SMI.
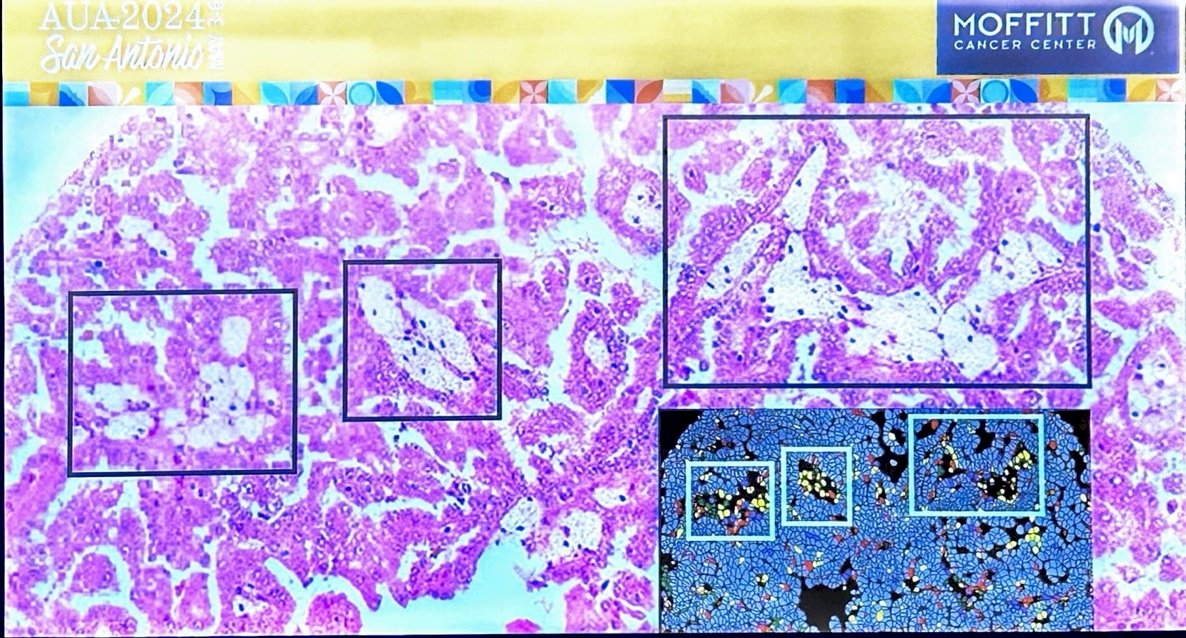
Figure 3. technique and results from using spatial transcriptomic through SMI.

Figure 4. technique and results from using spatial transcriptomic through SMI.
Presented by: Mitchell Hayes, MD, Oregon Health and Science University, Portland, Oregon
Written by: Paul Piedras, B.S., University of California, Irvine, @piedras_paul on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 – Mon, May 6, 2024.
References:
- Arora RD, Limaiem F. Renal Clear Cell Cancer. In: StatPearls. Treasure Island (FL): StatPearls Publishing; January 1, 2023.


