(UroToday.com) The 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX between May 3 and May 6, 2024, was host to the advanced kidney cancer podium session (PD18). Dr. Alireza Ghoreifi presented the results of a comparative study of patients with renal cell carcinoma (RCC) who underwent nephrectomy (open or minimally invasive) following immune checkpoint inhibitor (ICI) therapy. This study used a multicentric dataset, including data from five high-volume US academic centers between 2015 and 2023 (Figure below). The primary goal of the study was to report the outcomes of minimally invasive (MIS) nephrectomy following ICI therapy.
Dr. Ghoreifi initiated his presentation by illustrating the evolving timeline of systemic therapy options over the past two decades. Despite the availability of level 1 evidence endorsing the use of immune checkpoint inhibitors (ICI) either as monotherapy or in combination with targeted therapy for advanced RCC, there remains a scarcity of data regarding the outcomes of nephrectomy subsequent to ICI treatment, especially through a minimally invasive surgical (MIS) approach.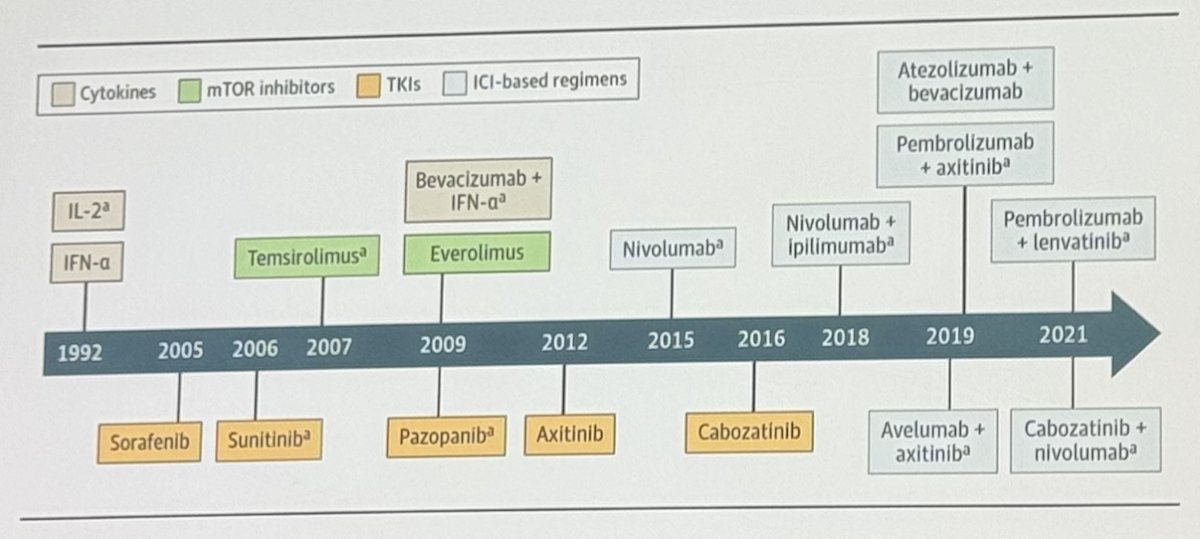
This analysis comprised 158 patients diagnosed with locally advanced or metastatic RCC, with 76 undergoing MIS and 82 undergoing open nephrectomies. Within the MIS nephrectomies, 56 were robotic operations and 20 were laparoscopic. Notably, the MIS cohort had a lower proportion of advanced RCC cases compared to the open cohort (64% vs. 84%). Furthermore, in the open cohort, 38% of patients presented with IVC thrombus, whereas only 11% did in the MIS cohort. The median age was 65 years in the MIS cohort and 62 years in the open cohort. Additional clinical and demographic characteristics are detailed in the table below. 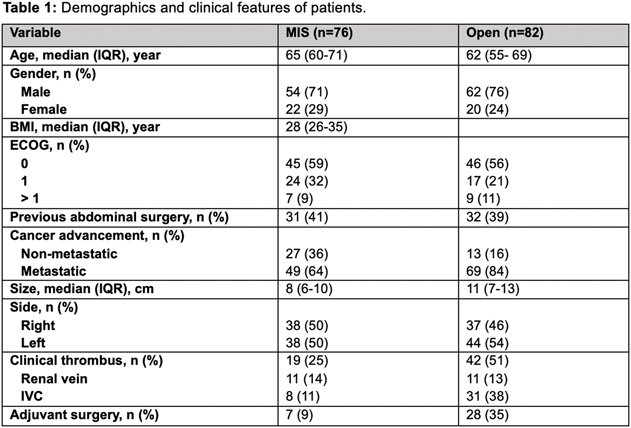
Among patients undergoing MIS nephrectomy, 6 individuals (8%) required conversion to open surgery, four robotic cases, and 2 laparoscopic procedures. Reasons for conversion included pancreatic injury in one patient, vascular injury in another, and failure to progress in four patients. Compared to patients undergoing open nephrectomy, those treated with MIS had lower median estimated blood loss (100 vs. 600 ml), shorter operative time (180 vs. 255 min), reduced length of stay (2 vs. 5 days), and lower rates of ICU admission (8% vs. 34%). Additionally, the 90-day complication rate was 22% in the MIS group compared to 35% in the open group, and the 90-day readmission rate was 9% in the MIS group vs. 13% in the open group. 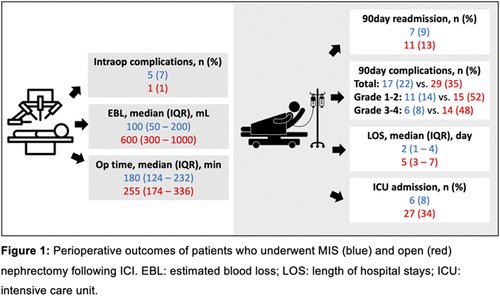
On multivariable analysis, they found that patients with non-metastatic RCC, as opposed to metastatic RCC (HR 3.1, 95% CI 1.3–7.3, p=0.01), smaller tumor size (HR 1.2 for each cm, 95% CI 1.1–1.3, p=0.001), and absence of clinical evidence of inferior vena cava thrombus (HR 29, 95% CI 3.5–237.4, p=0.002), were more likely to undergo minimally invasive surgery (MIS) instead of an open approach.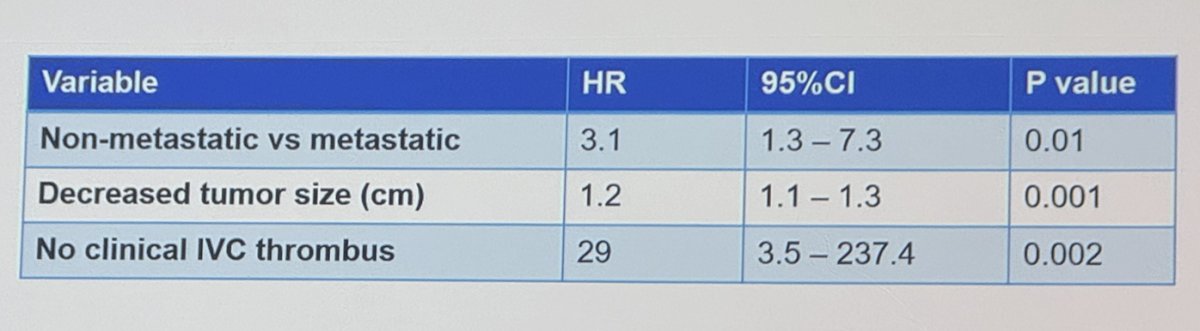
Dr. Ghoreifi presented that propensity score matching was utilized to weight data based on cancer advancement, tumor size, and clinical IVC thrombus. The table below displays patient characteristics before and after propensity score matching, with 70 patients in the MIS group matched to 45 in the open nephrectomy group.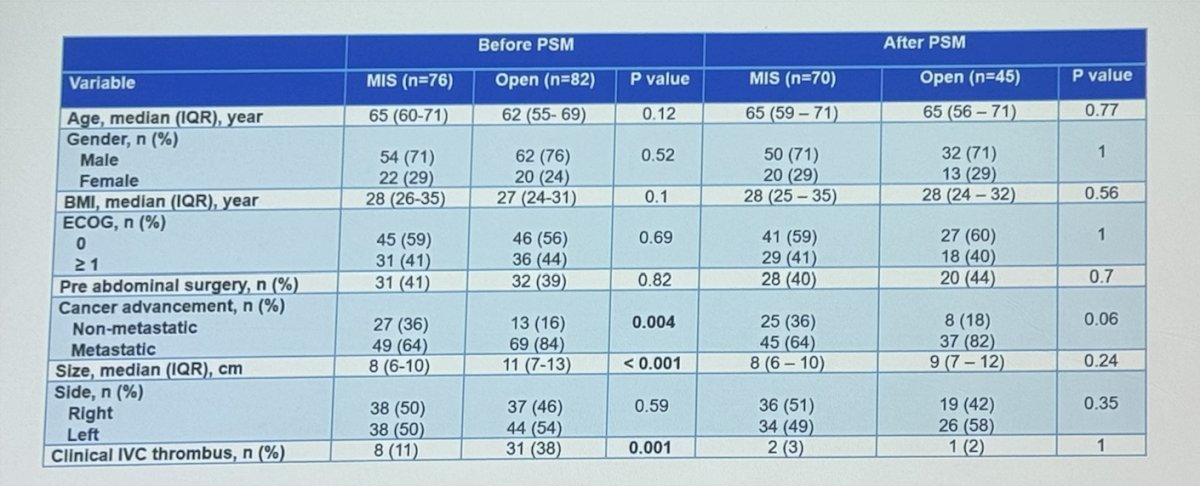
After propensity score matching, significant differences were found in median estimated blood loss (p<0.001), operative time (p=0.005), intraoperative transfusion (p<0.001), adjuvant surgery (p=0.006), length of stay (p<0.001), and ICU admission rate (p=0.009), all favoring the MIS approach.
Dr. Ghoreifi wrapped up his presentation with the following messages:
- The indications for nephrectomy in a post-ICI setting largely mirror those in treatment-naïve cases. However, certain cases may present added challenges, requiring careful preparation.
- Minimally invasive nephrectomy seems to be a safe option for appropriately selected patients with advanced or locally advanced renal cell carcinoma who are slated for nephrectomy after ICI therapy.
Presented by: Alireza Ghoreifi, MD, Research Fellow of Urologic Oncology, University of Southern California, Los Angeles, CA
Written by: Julian Chavarriaga, MD - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @chavarriagaj on Twitter during the 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX between May 3rd and May 6th, 2024


