(UroToday.com) The 2024 American Urological Association (AUA) annual meeting featured a session on overactive bladder, and a presentation by Dr. David Sheyn discussing long-term dementia risk with the use of anticholinergic versus beta-3-agonist pharmacotherapy for overactive bladder.
Anticholinergic medications are among the most frequently utilized treatments for overactive bladder, and there is increasing evidence to suggest that anticholinergic medications are associated with an increased risk of dementia by up to 1-5%. Some studies suggest that certain anticholinergic medications are safer than others due to their pharmacologic properties. However, existing literature for assessing beta-3-agonists has been limited by the following: a focus on oxybutynin and tolterodine, failure to include total anticholinergic burden as a confounder, lack of accounting for sex-based differences in dementia risk among patients with overactive bladder, and adjustment for selection bias. The objective of this study presented at AUA 2024 was to evaluate the risk of dementia in patients on anti-cholinergic medications while adjusting for these limitations.
This was a retrospective study using data from the TrinetX database of patients (11.2 million patients) prescribed either a beta-agonist or an anti-cholinergic medication for at least 3 months and within 1 year of an overactive bladder diagnosis beginning in 2012 and a follow-up of a minimum of 1 year. Medication use was assessed by evaluating prescriptions of specific medications with the inclusion of those who had two consecutive prescriptions at least 3 months apart. Patients with a diagnosis of pre-existing dementia or neurologic condition were excluded. Those who switched medications within class or between classes were also excluded. The primary outcome was an incident of dementia occurring >=12 months following the initiation of pharmacotherapy of anticholinergic medications.
Dementia was ascertained by either an ICD code or by prescription of galantamine, rivastigmine, tacrine, or memantine. Additional variables collected were age at overactive bladder diagnosis, sex, Elixhauser comorbidity score, and anti-cholinergic burden. Patients were divided into three groups: beta-3 agonists, low-risk anticholinergic (darifenacin, fesoterodine, tospium), and high-risk (oxybutynin, tolterodine, and solifenacin). To reduce confounding caused by age at index, sex, comorbidity, and anti-cholinergic burden, weights were included in the Kaplan Meier survival analysis and Cox proportional regression models. To account for selection bias, inverse probability of treatment weighting (IPTW) was performed.
During the study period, 136,621 patients met the criteria for inclusion, with 20,884 receiving beta-agonist, and a mean follow-up time of 4.3 +/- 2.5 years. Overall, 67.9% of patients were female, the most common race was white (69.3%), and the most common overactive bladder medications were oxybutynin (51.0%), mirabegron (17.3%), solifenacin (14.4%), and tolterodine (10.8%). The full baseline characteristics of the cohort are as follows: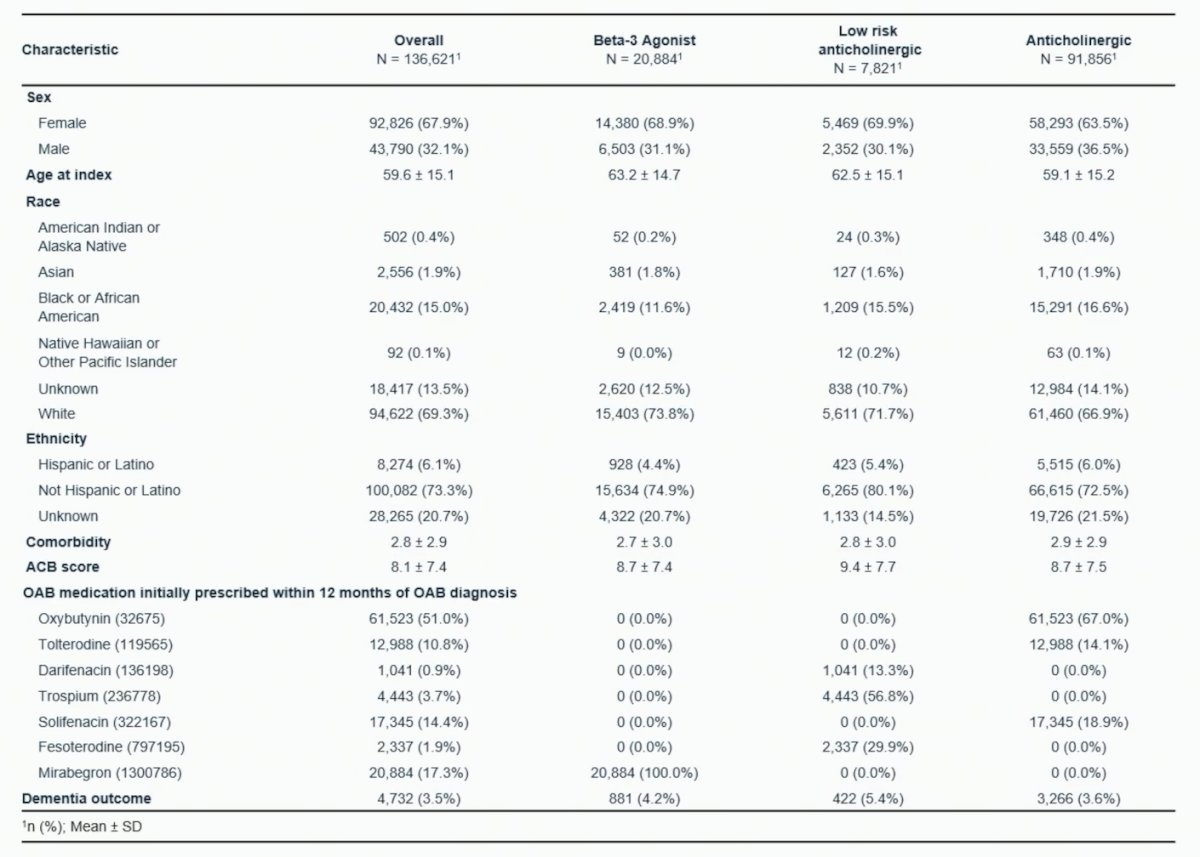
After adjusting for confounders, only oxybutynin (HR 1.12, 95% CI 1.00-1.26) was associated with an increased risk of dementia in women >65 years old relative to mirabegron, while in men, anti-cholinergic medications were associated with lower or no risk of dementia: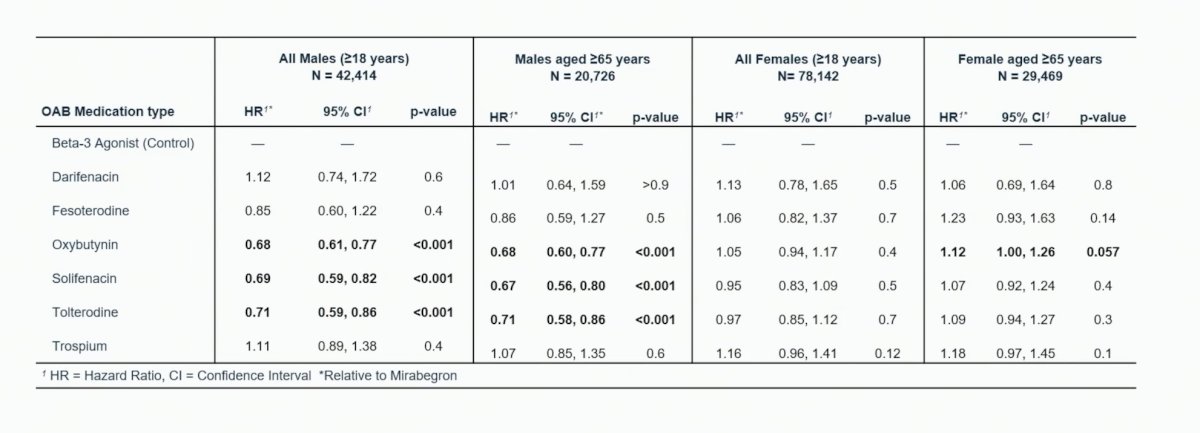
Dr. Sheyn concluded his presentation by discussing long-term dementia risk with the use of anticholinergic versus beta-3-agonist pharmacotherapy for overactive bladder with the following take-home messages:
- After accounting for sex, pre-existing conditions, medication type, and anticholinergic burden, only oxybutynin was associated with a 12% increased risk of dementia in women >= 65 years of age relative to mirabegron
- In men, anticholinergic medications were associated with a lower risk of dementia relative to mirabegron
- These findings may be a reflection of differences in the disease processes presenting as overactive bladder and the differences in dementia risk between men and women
- Further study into the etiology of overactive bladder symptoms in men and women and sex-based differences related to dementia will increase our understanding of both conditions
Presented by: David Sheyn, MD, Associate Professor of Urology and Reproductive Biology, Case Western Reserve University School of Medicine, Cleveland, OH
Written by: Zachary Klaassen, MD, MSc - Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 - Mon, May 6, 2024.


