(UroToday.com) The 2024 American Urological Association (AUA) Annual Meeting held in San Antonio, TX between May 3rd and 6th, 2024 was host to an advanced prostate cancer podium session. Dr. Stacy Loeb presented a sub-analysis of the IMPLEMENT study evaluating differences in barriers and facilitators to first-line treatment intensification in metastatic castration-sensitive prostate cancer (mCSPC) between urologists and oncologists.
First-line treatment intensification (i.e., androgen-deprivation therapy [ADT] plus chemotherapy, androgen receptor pathway inhibitors, or both) for mCSPC patients is recommended by international guidelines. These combination approaches have demonstrated improved overall survival outcomes, without affecting quality of life outcomes compared to ADT alone or in combination with non-steroidal anti-androgens. However, treatment intensification remains underutilized in real world practices, with only 13% and 37% of patients treated by urologists and medical oncologists, respectively, receiving such therapy.1 As such, the objective of this study was to examine differences in barriers and facilitators to mCSPC treatment intensification between urologists and oncologists using an implementation science approach.
In this study, Dr. Loeb and colleagues recruited 18 US-based urologists and oncologists who all treated ≥1 patients with mCSPC in the preceding 6 months and spent ≥50% of their time in direct patient care. They underwent virtual double-blind, semi-structured interviews using a Theoretical Domain Framework (TDF)-based discussion guide. TDF v1.0 consists of 12 domains; however, the Nature of Behavior domain was not included in this study because it describes the behavior rather than what influences the behavior. These interviews were transcribed, and quote coded into 11 TDF domains. Themes were generated within the domains and were subsequently evaluated to identify key barriers and facilitators. The impact of each theme on treatment intensification was scored based on an assessment by the research team. Divergence was scored according to the degree of conflicting beliefs within a theme. Numerical values were assigned to each parameter and summed to calculate the total score for net prioritization. A 20% difference was chosen for notable differences as it was previously established to be appropriate for an N = 18 sample upper bound on a 90% binomial confidence interval. The study design is illustrated below: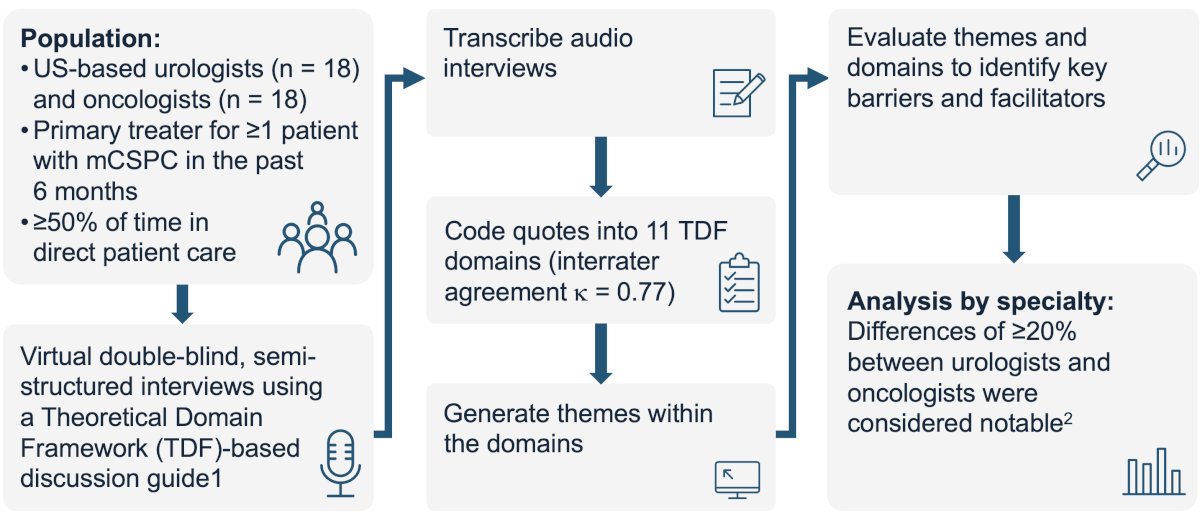
The participants characteristics are summarized below. Purposive sampling was used to obtain a diverse sample. The average years in practice was 21 for urologists and 16 for oncologists. 33% of urologists and 56% of oncologists were considered high intensifiers (i.e., intensify ≥50% of patients). The majority worked in a non-academic setting (72% and 50%, respectively).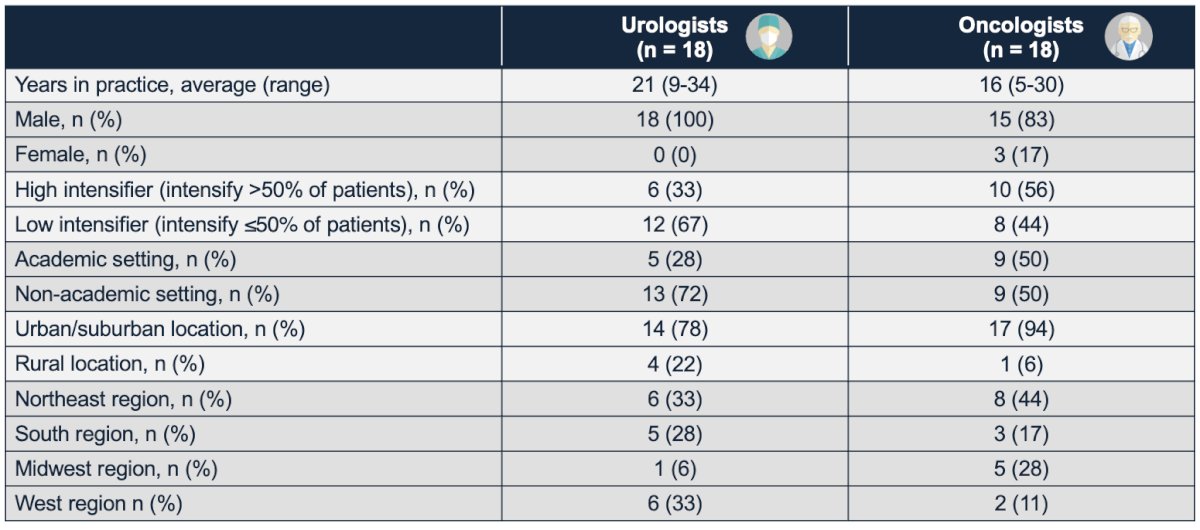
What were the key barriers identified in both specialties? In the ‘knowledge’ domain, “lack of knowledge regarding treatment intensification outcomes” was the most common barrier to treatment intensification implementation. 39% of urologists and 22% of medical oncologists stated their belief that “there is insufficient treatment intensification data”. Other common barriers included “waiting to intensify treatment second line” and “using first-line treatment intensification only for severe disease”.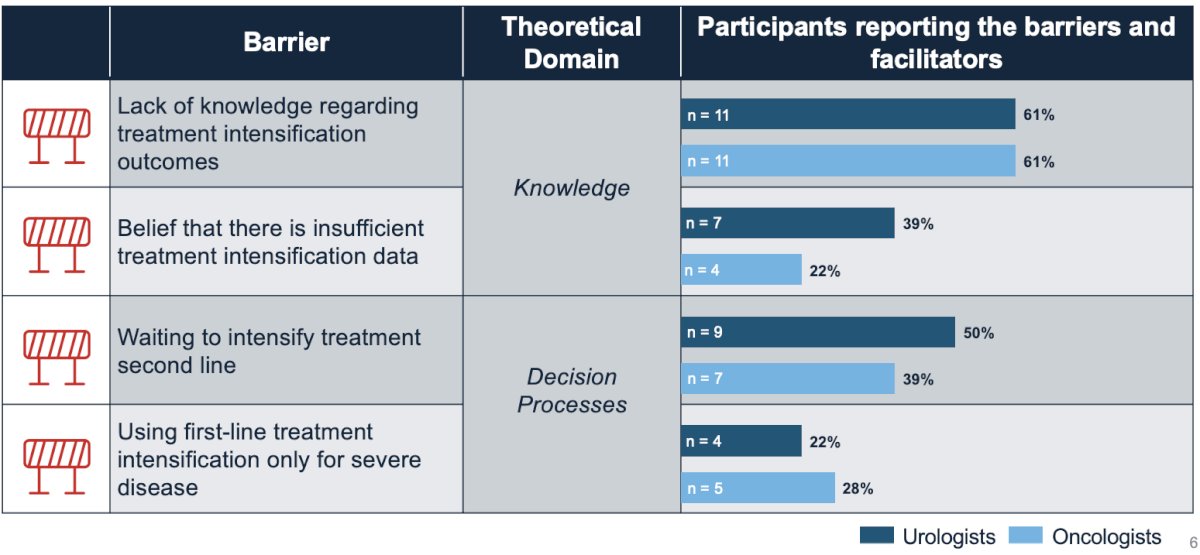
Conversely, facilitators to treatment intensification included “confidence in first-line treatment intensification” and “comfort with managing treatment intensification”.
What were notable differences in the key barriers and facilitators between specialties? The following facilitators were significantly more prevalent among urologists:
- Good interdisciplinary collaboration: 61% versus 39%
- Referring patients to an oncologist when intensification is not possible at practice: 50% versus 0%
- Belief that urologists should be able to intensify treatment: 56% versus 17%
“Urologists waiting too long to refer patients to oncologists” was a notable barrier per oncologists (28% versus 6%).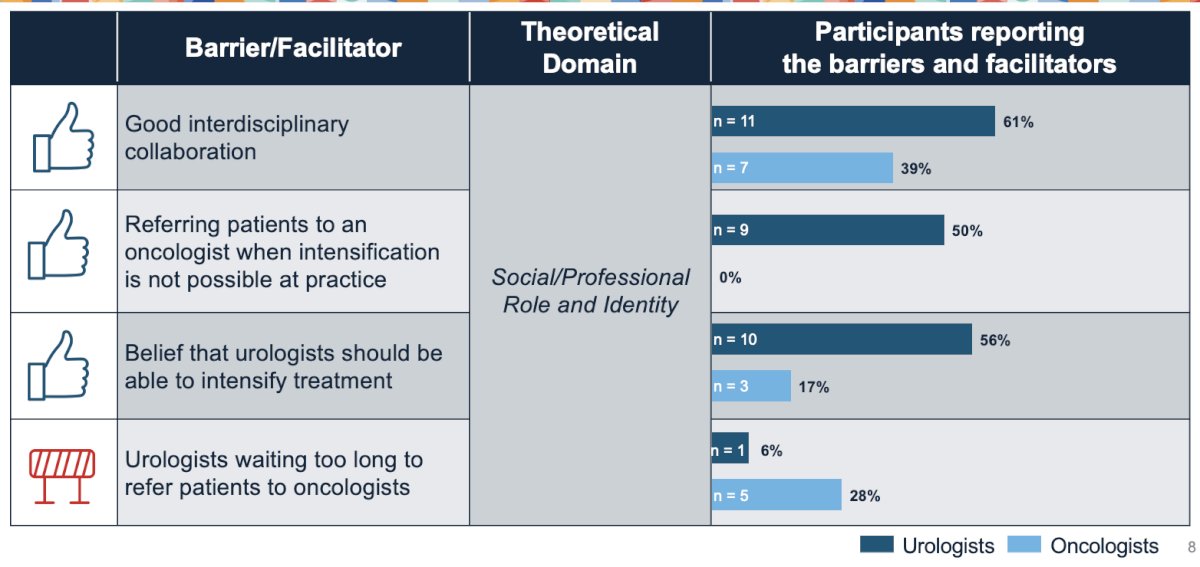 Conversely, the following facilitators were significantly more prevalent among oncologists:
Conversely, the following facilitators were significantly more prevalent among oncologists:
- Not limiting intensification based solely on age or performance status: 94% versus 72%
- Sufficient clinical support: 61% versus 39%
Urologists were significantly less likely to prescribe treatment intensification due to the following factors:
- Habit of not intensifying treatment 1st line
- Insufficient clinical support
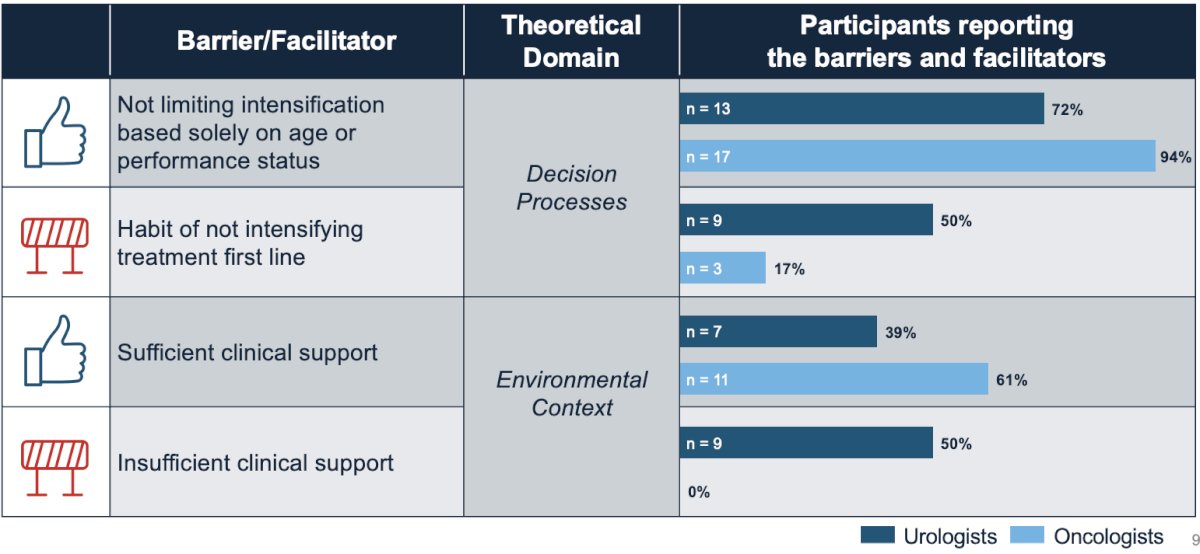
Notable differences in key and peripheral barriers and facilitators between specialties are summarized below: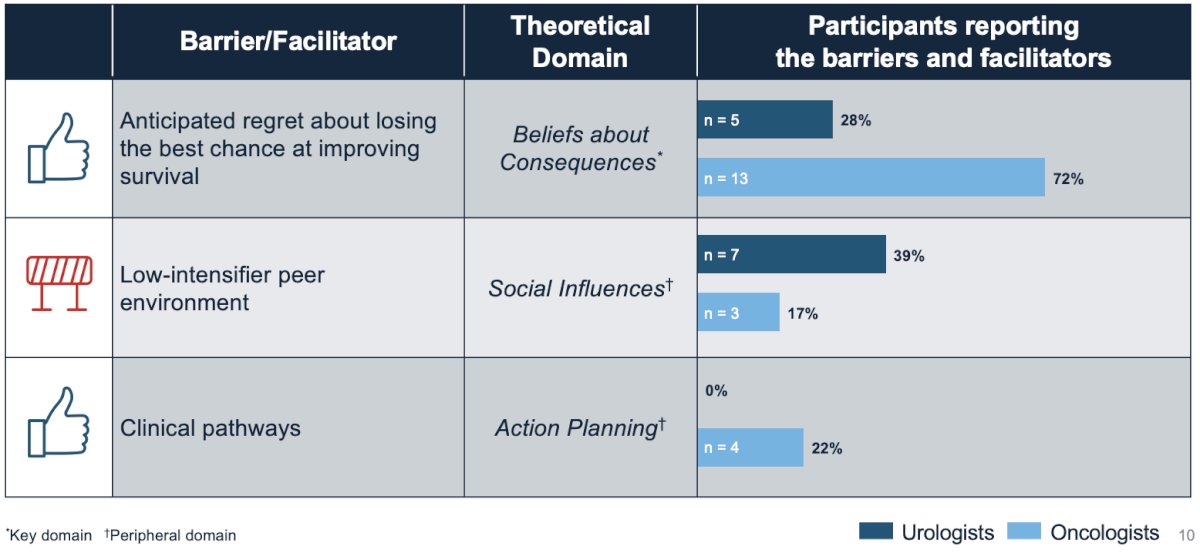
Dr. Loeb concluded her presentation by noting that common barriers/facilitators to treatment intensification in clinical practice include:
- Knowledge gaps
- Tendency to intensify second line and use first-line intensification only for severe disease
- Confidence in and comfort with first-line treatment intensification
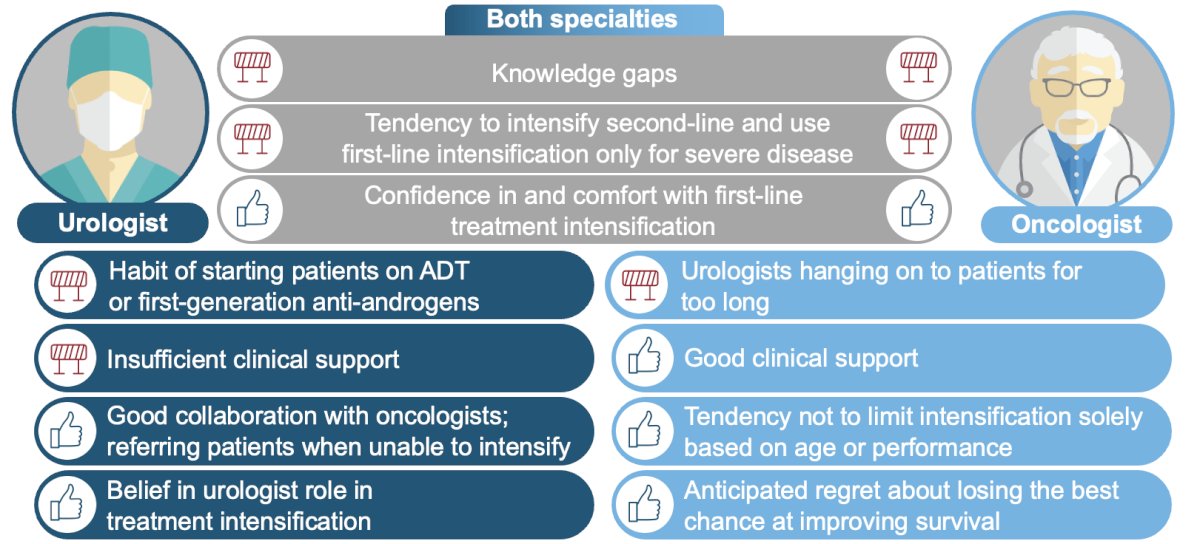
Intensification experiences between urologists and oncologists are very different and may explain the differences in intensification rates observed in published studies. These differences in barriers and facilitators must be addressed and leveraged, respectively, to provide optimal care for mCSPC patients.
Presented by: Stacy Loeb, MD, Professor of Urology and Population Health at NYU Langone Health and the Manhattan Veterans Affairs, New York, NY
Written by: Rashid Sayyid, MD, MSc - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, May 3rd - 6th, 2024
References:

